JACC:高温瑜珈导致急性心肌梗死1例
2014-04-08 清热解毒2号 dxy
高温瑜珈作为一种特殊的练习方法在全世界有成千上万的追随者,在加热(38℃-40℃)加湿的练功房内完成,一共26个姿势。有报告显示,过度劳累有可能引发斑块破裂和急性冠脉综合征(ACS)。美国加州MIKKON养生学院首席瑜伽导师说:“练高温瑜伽小心副作用。”高温环境里做动作会增加心脏的负担,会给高血压、低血压、糖尿病等慢性病患者带来严重后果(来自互动百科)。近日,西班牙学者Carlos Ferrera
高温瑜珈作为一种特殊的练习方法在全世界有成千上万的追随者,在加热(38℃-40℃)加湿的练功房内完成,一共26个姿势。有报告显示,过度劳累有可能引发斑块破裂和急性冠脉综合征(ACS)。美国加州MIKKON养生学院首席瑜伽导师说:“练高温瑜伽小心副作用。”高温环境里做动作会增加心脏的负担,会给高血压、低血压、糖尿病等慢性病患者带来严重后果(来自互动百科)。
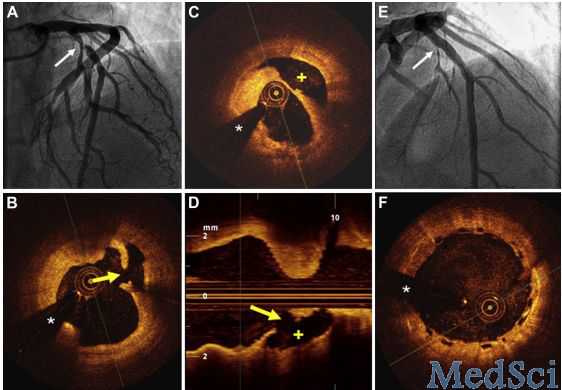
患者男,53岁,练习高温瑜伽时出现ST段抬高型急性冠脉综合征,既往无任何心血管危险因素。后予静脉内溶栓成功,溶栓后第1日行冠状动脉造影,发现左前降支动脉近端临界狭窄(图A箭头处),光学相干断层扫描(OCT)发现有斑块破裂(图B箭头处),并有一残腔(图C +)返流(图D)。
植入生物可降解支架1枚后,血管腔通畅,造影未见狭窄(图E)。光学相干断层扫描显示支架扩张良好,贴壁良好(图F)。患者住院期间安稳无恙,于4天后出院。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JACC#
19
#ACC#
26
#高温#
25
太狠了,这也可以作病例报道!
108