J Antimicrob Chemother:口服康泰克唑烷治疗成人复杂皮肤和软组织感染的效果不劣于与利奈唑胺
2022-07-03 MedSci原创 MedSci原创
Contezolid(康特唑烷)是一种新型的噁唑烷酮类抗菌剂,用于治疗由需氧和厌氧革兰氏阳性菌引起的感染,包括耐甲氧西林菌株。
Contezolid(康特唑烷)是一种新型的噁唑烷酮类抗菌剂,用于治疗由需氧和厌氧革兰氏阳性菌引起的感染,包括耐甲氧西林菌株。近日,发表于 J Antimicrob Chemother的一项III期、多中心、随机、双盲、主动对照试验评估了康特唑烷与利奈唑胺在成人复杂皮肤和软组织感染(cSSTIs)中的疗效和安全性。
研究纳入患有cSSTI的成人患者,按1:1的比例随机接受康特唑烷800 mg或利奈唑胺 600 mg q12h,持续7-14天。在全面分析组(FAS)和临床可评估组(CE)的治愈测试(TOC)访问中评估临床治愈率和安全性。非劣效性被定义为临床治愈率的治疗差异的95%CI下限大于-10%。
结果,TOC时的临床治愈率表明,在可临床评估的FAS以及FAS和CE人群中,康特唑烷800 mg q12h的治疗效果不劣于利奈唑胺600 mg组:92.8%(271/292)vs.93.4%(284/304)(差异-0.6%,95%CI:-4.7%至3.5%),81.4%(271/333)vs.84.5%(284/336)(差异-3.1%,95%CI:-8.8%至2.6%),90.5%(267/295)vs.90.1%(282/313)(差异0.4%,95%CI:-4.3%至5.1%)。康特唑烷和利奈唑胺对由甲氧西林敏感或甲氧西林耐药金黄色葡萄球菌引起的cSSTIs显示出相似的疗效。与利奈唑胺相比,康特唑胺治疗组白细胞减少症(0.3% vs.3.4%)和血小板减少症(0% vs.2.3%)的发生率明显降低。两组之间的治疗突发不良事件的发生率相当。
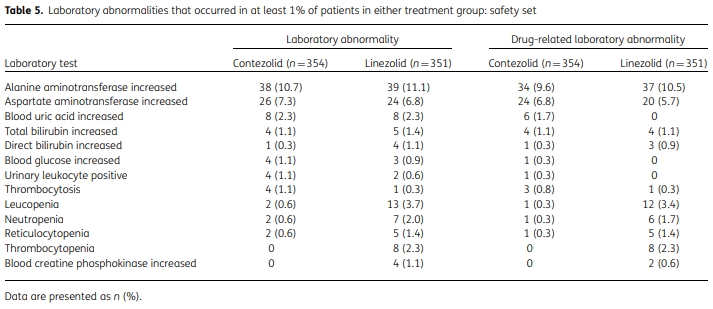
综上所述,该研究结果表明,康特唑烷800 mg q12h治疗成人cSSTIs与利奈唑胺一样有效,但在血液学不良事件方面比利奈唑胺更安全。
原始出处:
Xu Zhao, et al., A Phase III multicentre, randomized, double-blind trial to evaluate the efficacy and safety of oral contezolid versus linezolid in adults with complicated skin and soft tissue infections. J Antimicrob Chemother. 2022 May 29;77(6):1762-1769. doi: 10.1093/jac/dkac073.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#CRO#
40
#Micro#
49
#利奈唑胺#
41
#软组织#
40