Clin Cancer Res:局部晚期直肠癌的新治疗方案——术前放化疗联合纳武单抗巩固继以根治性手术!
2022-02-10 Nebula MedSci原创
术前放化疗后予以纳武单抗巩固治疗或可提高局部晚期直肠癌的病理完全缓解率
术前放化疗(CRT)加手术切除是局部晚期直肠癌(LARC)的标准治疗方法。将免疫检查点抑制剂与放疗相结合或有望提高这类患者的治疗效果。
本研究评估了术前放化疗后加用纳武单抗继以手术对局部晚期直肠癌患者的疗效。
这是一项 I-II 期的临床试验,在 I 期阶段,调查了序贯使用术前放化疗、5个疗程的纳武单抗和根治性手术的可能性;在 II 期阶段,评估了该治疗方案在微卫星稳定(MSS)和微卫星不稳定性高(MSI-H)的局部晚期直肠癌患者中的有效性。
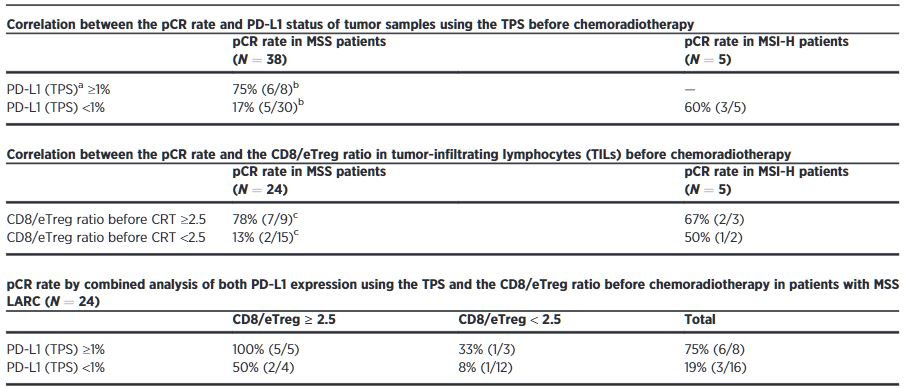
不同分组患者的病例完全缓解率
在 I 期,有3位患者接了全计划的术前放化疗和纳武单抗(无剂量调整);因此该方案被推荐用于 II 期阶段。MSS队列和探索性MSI-H队列患者的病理完全缓解率分别是30%(11/37, 90% CI 18%-44%)和60%(3/5)。虽然有3位患者经历了与免疫相关的严重不良反应,但无与治疗相关死亡。
在38位进行了手术治疗的MSS患者中,程序性细胞死亡配体1(PD-L1)肿瘤比例评分≥1%和<1%病理完全缓解率为75%(6/8)和 17% (5/30; p=0.004)。
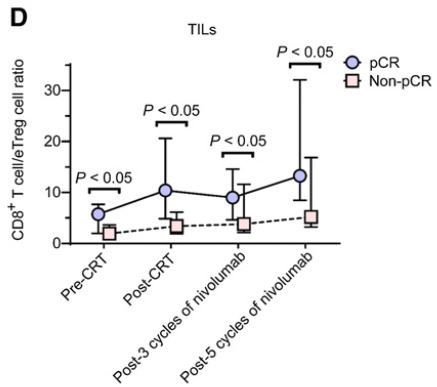
治疗过程中,CD8/eTreg 细胞比例的变化
在24位MSS患者中,采用流式细胞术分析放化疗前的样本,肿瘤浸润CD8+ T细胞/效应调节T细胞(CD8/eTreg)比例≥2.5和<2.5的患者的病理完全缓解率分别是78%(7/9)和13%(2/15,p=0.003)。
总之,术前放化疗后予以纳武单抗巩固治疗或可提高局部晚期直肠癌的病理完全缓解率。PD-L1表达和CD8/eTreg比例升高都是微卫星稳定的局部晚期直肠癌患者的阳性预测指标。
原始出处:
Hideaki Bando, Yuichiro Tsukada, Koji Inamori, et al. Preoperative Chemoradiotherapy plus Nivolumab before Surgery in Patients with Microsatellite Stable and Microsatellite Instability–High Locally Advanced Rectal Cancer. Clin Cancer Res February 7 2022 DOI:10.1158/1078-0432.CCR-21-3213.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#治疗方案#
62
#局部晚期直肠癌#
35
#根治性手术#
31
#局部晚期#
0
新技术,有用
45
新方法,值得推广
45
#放化疗#
41
#局部#
35
#根治#
40