JCEM:有妊娠期糖尿病病史妇女发病率的长期随访
2022-08-28 从医路漫漫 MedSci原创
妊娠期糖尿病的患病率在全球范围内不断上升,使妊娠期糖尿病成为妊娠最常见的医学并发症。
背景:妊娠期糖尿病的定义是在怀孕期间诊断出的异常糖耐量,在丹麦,这是一种使大约5%的妊娠复杂化的疾病,与欧洲其他地区以及澳大利亚和北美(2)报告的2%-9%的怀孕情况一致。最近的几项研究表明,妊娠期糖尿病的患病率在全球范围内不断上升,使妊娠期糖尿病成为妊娠最常见的医学并发症。在大多数女性中,葡萄糖耐量在分娩后几天内恢复正常。有妊娠期糖尿病病史的女性在晚年患糖尿病(DM)的风险显著增加,尤其是2型糖尿病(T2 DM)。众所周知,T2 DM与发病率和死亡率的增加有关,例如,心血管事件,如心肌梗死、心脏和肾功能衰竭。因此,有妊娠期糖尿病病史的妇女患心血管疾病和心力衰竭的风险也显著增加,这也就不足为奇了,因为高血压和高脂血症的发生率已经在生育年龄。
然而,人们对其他类型发病率的风险知之甚少,例如有妊娠期糖尿病病史的妇女患上癌症。基于对患有妊娠期糖尿病的妇女8年的平均随访的研究表明,与没有妊娠期糖尿病的妇女相比,患甲状腺癌的风险增加,但绝经前乳腺癌的风险降低。在19年的随访中,非酒精性脂肪性肝病的发展也与妊娠期糖尿病的病史显著相关。大多数研究没有超过10年的随访,因此,除了T2 DM和心血管疾病之外,妊娠期糖尿病可能产生的长期后果的描述很少。
目的:因此,本系统回顾的目的是调查与其他妇女相比,有妊娠期糖尿病病史的妇女是否有1)独立于T2 DM和心血管疾病的慢性疾病的长期风险增加;以及2)过早死亡的长期风险增加。该综述仅限于妊娠合并妊娠期糖尿病后平均随访期至少为10年的研究。
方法。基于截至2021年3月31日在Medline、Embase和Cochrane Library中的搜索,使用广泛的关键词进行系统综述。我们提取了有关GDM与产后至少10年的疾病发生率之间的相关性的研究特征和结果,排除了对妊娠前患有糖尿病或仅在结果前患有糖尿病的妇女的研究。根据系统综述和荟萃分析(PRISMA)的首选报告项目报告结果。纽卡斯尔-渥太华量表用于评估偏倚风险。
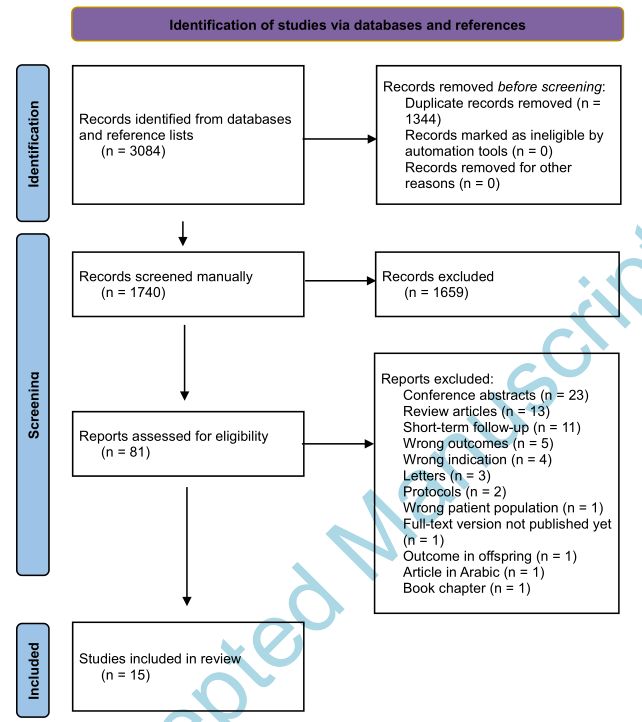
结果。我们筛选了3,084个标题,对81篇文章进行了全文评估,15篇纳入了综述。最有力的证据是肾脏疾病,尤其是黑人女性。我们发现了与肝病相关的迹象,可能仅限于产后T2DM的妇女。GDM和乳腺癌之间的联系已被广泛研究,但在大多数情况下是基于自我报告的诊断和相互矛盾的结果。对于其他癌症,只发现了稀疏和不一致的结果。没有发现关于甲状腺疾病的研究,也没有研究报道有GDM病史的妇女的短期或长期死亡率。
表1妊娠期糖尿病(GDM)病史与长期发病率之间的关系
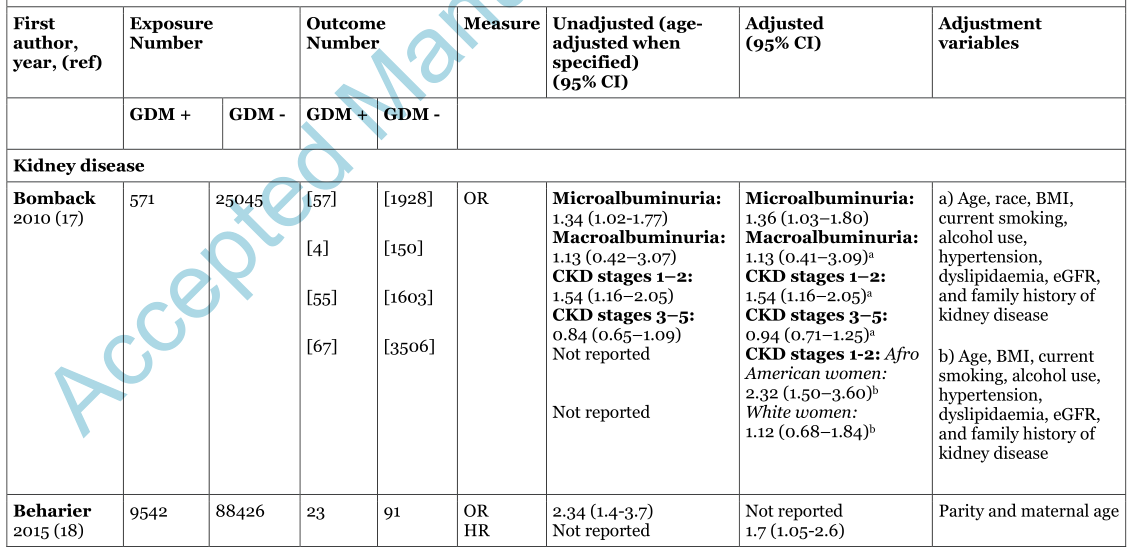
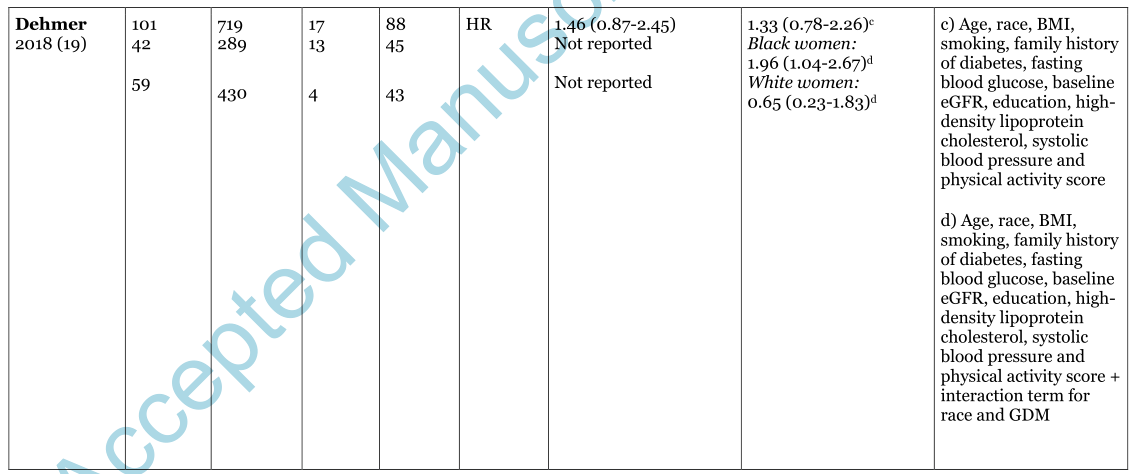


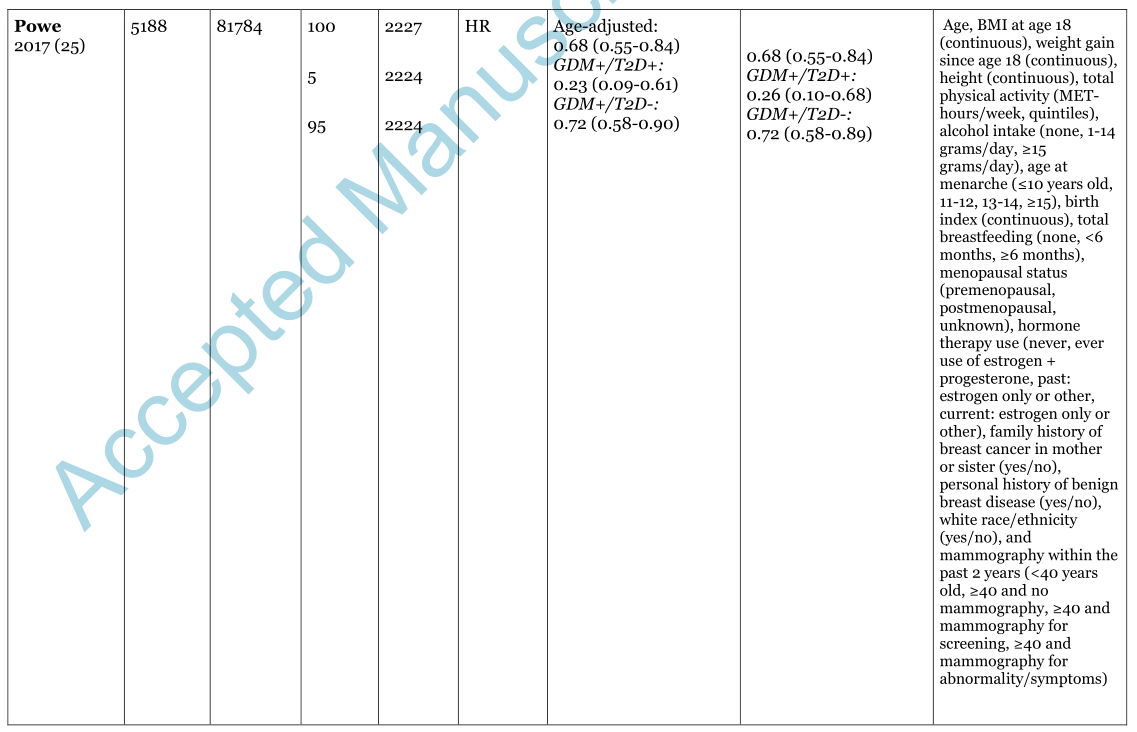


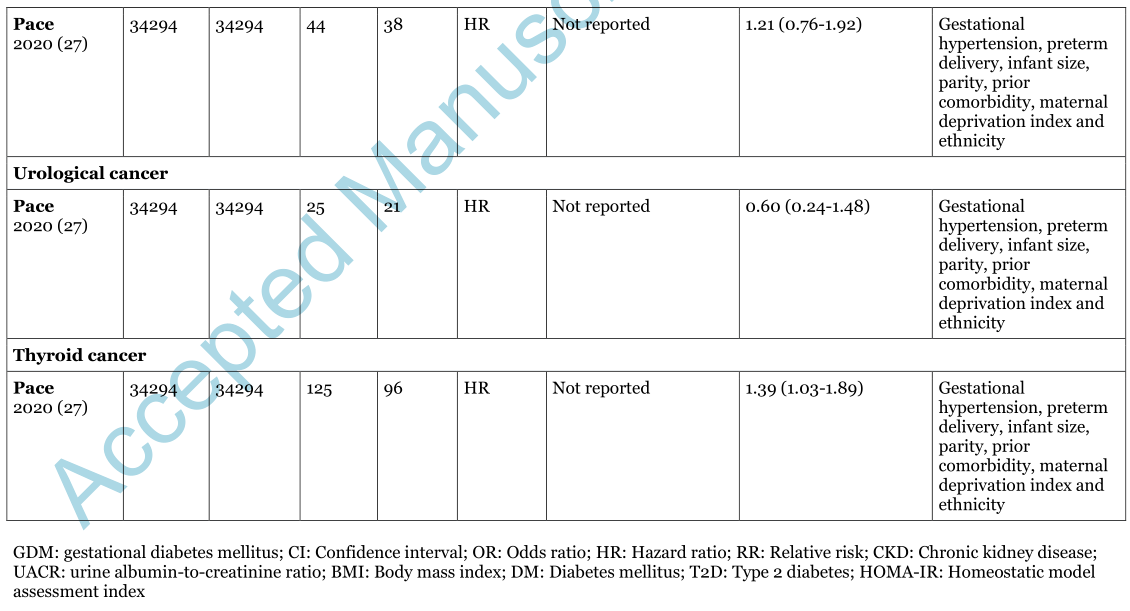
图1.文献检索和选择过程的流程图。
结论:鉴于GDM的频率,需要更好的证据证明可能的长期健康后果,特别是基于GDM诊断和长期健康结果的综合记录的研究。
原文出处:Flachs Madsen LR, Gerdøe-Kristensen S, Lauenborg J,et al.Long-Term Follow-Up on Morbidity Among Women With a History of Gestational Diabetes Mellitus: A Systematic Review.J Clin Endocrinol Metab 2022 Aug 18;107(9)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#长期随访#
45
#JCEM#
36
#JCE#
24
#发病率#
36
有意思
39
#妊娠期#
46
#妊娠期糖尿病#
55