INT J LAB HEMATOL:小细胞性贫血的鉴别诊断:小红细胞和低色素红细胞的作用
2017-04-13 MedSci MedSci原创
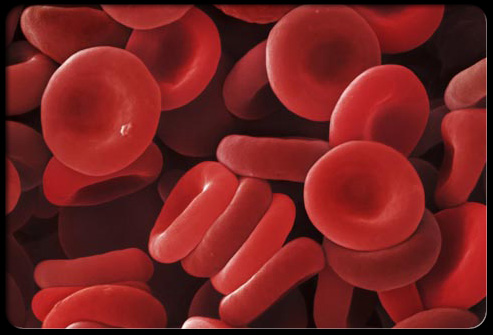
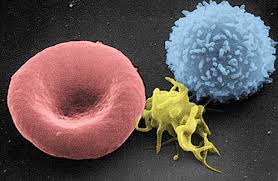
目前已经研究关于衍生自红细胞(RBC)参数的各种指标,用于区分地中海贫血和缺铁性贫血。该研究了小红细胞与低色素红细胞的比值作为小细胞性贫血的判别指标,并将其与传统指标进行比较,且在实验组中确证其中的发现。
近日,来自西班牙Galdakao Usansolo Galdakao医院血液科,的研究人员报道了一项关于小细胞性贫血的鉴别诊断的研究,相关研究成果刊登于国际杂志INT J LAB HEMATOL上。
目前已经研究关于衍生自红细胞(RBC)参数的各种指标,用于区分地中海贫血和缺铁性贫血。该研究了小红细胞与低色素红细胞的比值作为小细胞性贫血的判别指标,并将其与传统指标进行比较,且在实验组中确证其中的发现。
研究组包括来自371名小细胞性贫血症患者的样本,其平均细胞体积(MCV <80fL),在CELL-DYN蓝宝石分析仪上测量这些样本并计算各种判别函数。使用ROC分析建立最佳临界值。这些值用于338名患者的实验组。
研究显示,研究组中,小红细胞与低色素红细胞比> 6.4是明确指示地中海贫血(曲线0.948下的面积)。 Green-King和England-Fraser指数在ROC曲线下显示一致的面积。然而,小细与低色素的比率具有最高的灵敏度(0.964)。在实验组中,91.1%的小细胞性贫血患者能被M / H比正确分类。
总体而言,CELL-DYN蓝宝石测得的小红细胞与低色素红细胞比率与Green-King指数在识别地中海贫血携带者方面表现相同,但灵敏度更高,使其成为快速而廉价的筛选工具。
原始出处:
E. Urrechaga,J. J. M. L. Hoffmann,S.
Izquierdo,J. F. Escanero. et al. Differential diagnosis of microcytic anemia:
the role of microcytic and hypochromic erythrocytes. INT J LAB HEMATOL . DOI:
10.1111/ijlh.12289
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞性#
38
#色素#
27
#红细胞#
27
#EMA#
36
#鉴别诊断#
35