Chest:治疗脓毒症期间房颤——β受体阻滞剂优于CCBs
2016-01-09 fsy 译 MedSci原创
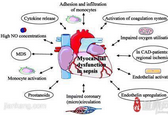
脓毒症期间发生房颤(AF)增加发病率和死亡率,但在脓毒症期间有针对性的治疗AF心率和节律的实践模式和结果目前还不清楚。该项回顾性队列研究的数据来自于约20%的美国医院。研究人员确定了脓毒症期间IV级AF治疗的相关因素(β受体阻滞剂[BBs],钙通道阻滞剂[CCBs],地高辛,或胺碘酮)。研究人员使用倾向得分匹配和工具变量的方法来比较不同治疗房颤方法之间的死亡率。在39693例脓毒症期间发生房颤的患
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Chest#
33
#EST#
36
#受体阻滞剂#
0
这篇文章有一定深度
139
是一篇不错的文章
127
#阻滞剂#
35
给力
108
谢谢分享,学习了
111
#β受体阻滞剂#
36
#CCB#
50