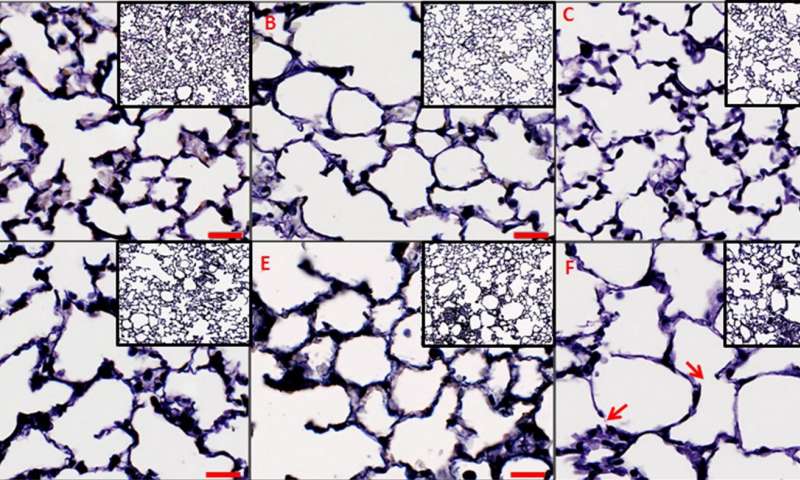
PLoS Comput Biol:研究揭示肺功能下降细节,或能“根除”慢性肺病!
2017-08-25 Heather_z727 来宝网
克里斯托弗·马萨罗格斯大学的科学家们开发出了一种新的虚拟模型,可以详细对照不同因素导致的慢性肺部疾病炎症的改变。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肺病#
37
#肺功能下降#
46
#根除#
24
#Biol#
23
#慢性肺病#
29
#Bio#
24
谢谢分享.学习了!
53
非常好的文章.学习了.很受益
57
学习了.谢谢分享
57
模型提供了一种新的方法用于检查病变肺功能改变.
56