有研究报道,下呼吸道感染后儿童患哮喘风险增加,但很少有研究专门评估婴儿期诊断为肺炎的儿童的哮喘风险。此外,但尚不清楚这种关联是否存在因果关系,或者某些儿童是否存在两种疾病的易感性。
发表在CHEST杂志的一篇文章评估婴儿期肺炎与4岁哮喘之间的相关性,同时控制遗传和家族混杂因素;并评估婴儿期肺炎与4岁时哮喘之间相关性是否在接种肺炎球菌结合疫苗(PCV)后发生了改变。

研究纳入2001年7月至2010年12月间出生的瑞典儿童,共948045名,其中23086 (2.4%)例儿童2岁前被诊断为肺炎。与未患肺炎儿童相比,诊断为肺炎的儿童中男性、早产、剖宫产、小于胎龄儿、母亲孕期吸烟、合并症、父母文化程度低和父母哮喘的比例较高。
婴儿期肺炎与4岁时哮喘患病风险有较强相关性(校正OR=3.38; 95%CI, 3.26-3.51),控制混杂因素后,点估计值变化不大(校正OR=2.81; 95%CI, 2.58-3.06)。与未接种肺炎球菌结合疫苗的婴儿相比,接种肺炎球菌结合疫苗的婴儿确诊肺炎后哮喘患病率的风险略高(校正OR=3.80, [95%CI, 3.41-4.24] vs 校正OR=3.28, [95%CI, 3.15-3.42]),而病毒性肺炎的病因比例较高(14.5% vs 10.7%),总体哮喘患病率较低(5.3% vs 6.6%)。
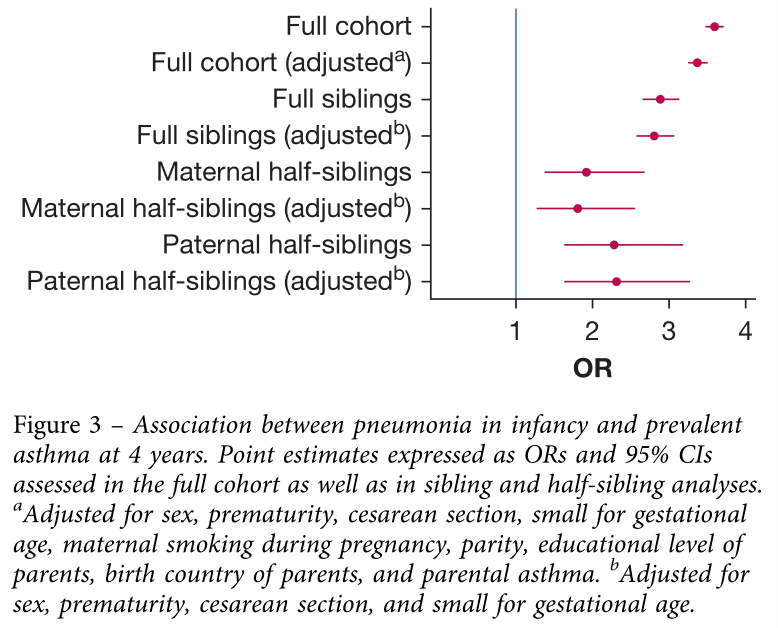
研究表明,尽管控制了遗传和家庭环境的混杂因素,婴儿期肺炎与4岁时患哮喘风险密切相关。如果这种相关性是因果关系,则意味着针对肺炎的干预措施会进一步获益。
原文出处:
Samuel Rhedin, Cecilia Lundholm, et al, Pneumonia in Infancy and Risk for Asthma, chest, 2021, https://doi.org/10.1016/j.chest.2021.03.006.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Chest#
33
#EST#
24
#患病风险#
31
#婴儿期#
32