吴强:规范经桡动脉途径(TRI)和经股动脉途径(TFI)入径选择对比及常见并发症预防处理
2020-12-31 《门诊》杂志 门诊新视野
介入治疗中,经桡动脉途径(TRI)和经股动脉途径(TFI)是两种常用的入径选择。临床中,指导广大介入医师熟悉两种入径的优劣之处以规范化手术入径的选择是具有切实意义的话题。
介入治疗中,经桡动脉途径(TRI)和经股动脉途径(TFI)是两种常用的入径选择。TFI作为冠脉介入的经典入路,临床应用广泛,而在复杂冠脉病变中,TRI因其安全性高、血管并发症少、患者住院时间短等优势已成为主流。临床中,指导广大介入医师熟悉两种入径的优劣之处以规范化手术入径的选择,同时减少两种入径常见并发症的发生并给予及时、有效的处理,是具有切实意义的话题。
TRI&TFI入径的选择之优劣
近百年来,介入医学技术发展道路中主要经历了三个“里程碑”;早在1953年,Sven-Iran Seldinger医生即创立了经皮血管穿刺技术,成为介入医学技术发展的起点,从此赋予介入医学“微创”的意义并沿用至今;1989年,Campeau报道了首例经桡动脉途径冠状动脉造影;而在1993年,Kiemeneij等人先后探讨并证实了经桡动脉途径行PTCA及支架置入的可行性,引起了学术界的普遍关注,随后TRI入径的介入治疗迅速在全球开展。
尽管TRI入径优势颇多备受推崇,其仍不能完全取代TFI,两者各有千秋,其适应症亦不相同,临床中选择哪种入径需介入医师综合考量患者实际情况后作出决策。从解剖结构来看,桡动脉较股动脉更细、迂曲更常见,且无重要的血管、神经伴行,因此TRI入径具备以下优缺:患者术后恢复快可立即行走,减少了住院时间、费用;外周血管、神经并发症少见,多适用于背部疾病及肥胖患者;无需血管封闭器,止血容易。其缺点一是术者会接触到大量射线,有害术者的健康;二是因桡动脉血管内径小,穿刺不易成功,血管提供的被动支撑小,导致其对器械要求较高,器械选择上往往受限,另则桡动脉迂曲时发生痉挛的情况十分常见。
TFI作为冠脉介入的经典入路,临床应用广泛,有着穿刺容易、无需特殊器材支持、血管内径大适用于各种介入器械的优势。缺点则在于TFI入径的患者术后需严格卧床、血管封闭器材费用高昂、操作不慎引起的局部血管及神经并发症多,如各种血管、神经病变及尿潴留等。
总的来说,TRI与TFI两种入径的优劣一定程度上呈互补之态,TFI适用性广但在预后方面不及TRI;TRI则更为安全、高效,但相对的器械要求较高,并更多地应用于复杂冠脉病变的患者。
桡动脉入径并发症及处理
桡动脉细小、易痉挛,且TRI入径的介入治疗中器械操作难度较高,介入医生的学习培养曲线更长。尽管熟练的操作可大幅提高介入的成功率,TRI入径的并发症仍不容忽视,其临床并发症主要为:
前臂疼痛或不适。临床表现为局部麻醉、穿刺、送入动脉鞘管、操纵导管及导丝、拔除动脉鞘管过程中,患者前臂有明显的疼痛和发胀感,停止操作后症状逐渐缓解;术后的前臂疼痛常与前臂血肿、血管闭塞、血管炎症相关;防治方面可通过充分的局部麻醉、操纵器械时注意动作轻柔、选择直径较小的导管等对策,降低前臂局部疼痛不适的并发症情况。
桡动脉痉挛。TRI入径最常见的并发症,发生率高,但可自行解除且一般没有远期不良后果。其病因是器械直接刺激血管,或是血管畸形、病变导致器械进入桡动脉分支,引起血管内皮儿茶酚胺水平的增高进而引发桡动脉的痉挛。危险因素方面涉及患者、术者以及器械三个方面,女性、糖尿病及吸烟患者,或血管径路解剖异常、手术时间延长的患者易发生桡动脉痉挛;术者穿刺时麻醉不充分、反复穿刺、动作粗暴等为重要诱因;器械方面,硬度大的导管、非亲水涂层的导管、导丝以及使用短的动脉鞘管将增加桡动脉痉挛的发生率。为预防桡动脉痉挛的发生,在术前应对患者进行充分的镇静、麻醉、应用扩血管药物,并为患者选择合适的器械,除此之外,术者轻柔精简的操作亦为关键;若桡动脉痉挛严重,手术无法进行时可考虑改用对侧桡动脉或股动脉入径;对于术后痉挛严重者,导丝、导管难以撤回的情况,可在持续给予扩张血管及镇静药物下待痉挛解除再拔除导管,或是采用臂丛神经麻醉后撤出导管的解决方案。
前臂血肿、前臂骨筋膜室综合征。前臂血肿多由反复穿刺或穿刺手法粗暴、不当引起桡动脉的撕裂、损伤;术后前臂血肿主要与术后加压包扎无效、不规范或提前减压有关;对于此种情况,术中的规范操作以及术后有效包扎止血是预防前臂血肿的关键。若前臂血肿较为严重,血液外渗至骨筋膜室则会继发为前臂骨筋膜室综合征,其临床表现为进行性疼痛,进一步可致坏疽、休克、肾功能衰竭等,严重者甚至需进行截肢处理。治疗方面在压迫止血、前臂制动的前提下,将肢体放置于心脏同水平面,密切关注肢端血运、感觉运动情况。一旦出现手部苍白、疼痛等缺血性症状时,应立即行筋膜间室切开进行减压。
桡动脉闭塞。东亚人群桡动脉内径一般约为2 mm,而小于2 mm的人群与鞘管无法匹配,糖尿病患者更是如此,此类人群易发生术后桡动脉闭塞,另有术前肝素的用量不当、术后穿刺点压迫时间过久也会引起桡动脉内形成栓塞。桡动脉闭塞的临床表现不明显,临床检查中桡动脉搏动消失,经绕动脉造影及超声检查发现血栓形成后,才可确诊。因桡、尺动脉共同循环,桡动脉的栓塞一般无特殊不良情况,可不予特殊处理,若血栓向肱动脉延伸则应及时进行溶栓治疗。
假性动脉瘤。一般情况下没有症状,只表现为局部出现搏动性肿块,体检可闻及血管杂音,彩超可见肿块内有血流信号,肿块的一端与动脉血管相通。治疗一般采用超声引导下压迫法,对于动脉瘤较大者可行超声引导下瘤腔内注射凝血酶、外科动脉修补术等。
非闭塞性桡动脉损伤。经TRI途径介入手术后有患者出现永久性的、非闭塞性桡动脉损伤,临床不常见,平均发生在术后4~5个月,诱发原因可能是操作中动脉鞘管和导管损伤血管内膜,引起内膜损伤性炎症。
穿刺点出血。桡动脉穿刺点下有桡骨提供支撑,利于局部压迫止血;桡动脉和尺动脉相互交通,穿刺点压迫止血要同时压迫穿刺点的近端和远端,避免因尺动脉的供血导致穿刺点出血或血肿形成。术后不注意腕部制动或围术期应用大量抗凝剂等,亦可导致穿刺点的局部出血、皮下淤斑,出血较多时可在局部及前臂形成血肿。
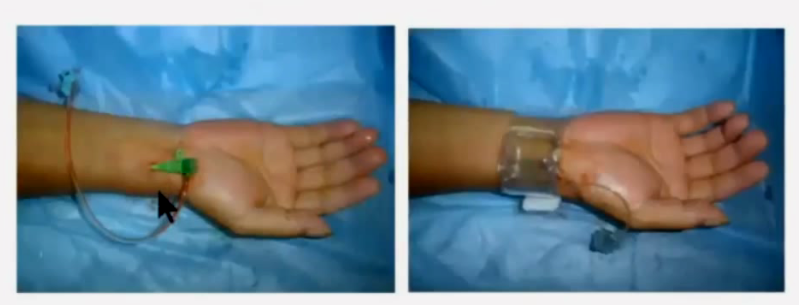
图1. 穿刺点出血处理
股动脉入径并发症及处理
TFI入径一般适用于TRI入径不适合或需要大腔下的Guiding进行冠脉操作的情况,临床并发症以出血、血肿最为常见(图2),同时后腹膜出血是其相对隐蔽的严重并发症,临床中应给予重视。股动脉入径常见并发症主要为:
出血、血肿。股动脉路径穿刺位点较低,同时大动脉鞘、鞘管置入时间长等因素引起的局部出血、水肿为主,处理原则为对可触及的血肿或可见性出血给予即刻压迫止血,同时开放静脉,进行扩容治疗或在必要时输血;可根据患者血肿情况,合理延长压迫止血的时间、判断是否停用抗栓药物并在必要时拮抗抗凝治疗。
假性动脉瘤。亦为TFI入径的常见并发症,临床表现为疼痛,可见局部肿大、搏动性团块并闻及血管杂音,其与TRI入径发生的假性动脉瘤的病因相似,主要由术后未进行有效加压或过早减压引起;防治方面,对于小于2 cm的小动脉瘤可维持观察,继续加压包扎;大部分动脉瘤可通过重新有效的加压包扎解决,对于动脉瘤巨大等极端情况可进行外科修补或超声指导下的凝血酶注射。
后腹膜出血。TFI入径的严重并发症且临床中难以及时发现,患者术后未见明显血肿,但出现贫血、低血压、腹部压痛、出汗等症状。处理原则分为三步走:(1)进行即刻处理,纠正抗凝治疗、给予扩容治疗并进行包扎压迫;(2)进行诊断,结合造影、CT评价血流动力学的稳定性;(3)进行病因治疗,改善腹壁下动脉栓塞问题,以制止后腹膜出血的进一步发展。
动静脉瘘。由于股动静脉相近,甚至呈上下交错的形态,进行穿刺时有可能静脉、动脉同时进入,若术后加压包扎不够充分则可能形成动静脉瘘。大部分动静脉瘘亦可在有效的局部压迫后自然闭塞,与假性动脉瘤相似,必要时可行外科修补。
神经损伤。TFI入径导致的神经损伤多由局部麻醉或穿刺、压迫、血肿等引起,通常累及股外侧皮神经,通常可自愈,不存在远期影响。
感染。主要由术中操作时间过长导致,并多见于糖尿病患者,临床可有发热表现,严重者可继发败血症、休克等危险症候,应及时进行抗感染治疗并给予患者对症处理。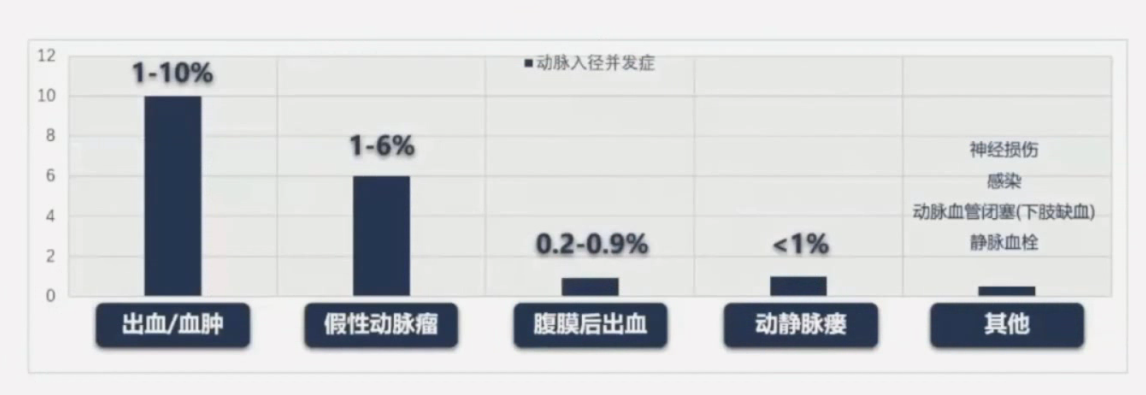
图2. 股动脉常见并发症临床发生率
总 结
动脉入路是冠脉介入诊疗的第一步,需要术者熟练掌握脉管系解剖、影像及器械的操作技巧,术中时刻关注患者的症状和生命体征,做好对鞘管的管理。同时也要熟悉抗栓、抗凝等相关药物的使用,方能在遇到问题时,做到有条不紊,保障患者的医疗安全。对于介入入路的相关并发症方面,“预防”是最高境界,一旦并发症发生,早期的识别和妥善处理尤为重要。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#并发#
36
#股动脉#
43
#经股动脉#
38
#经桡动脉#
43
#桡动脉#
46