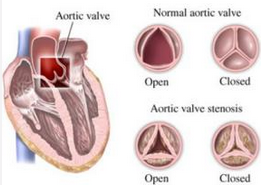
JACC:主动脉瓣狭窄女性怀孕有风险,受孕前需谨慎
2016-10-11 MedSci MedSci原创
在主动脉瓣狭窄(AS)女性中,目前关于母体风险和胎儿结果的报告结果都是有争议的。来自德国的研究人员开展了一项研究,作者试图在一个大型队列中调查AS患者的母体和胎儿结局。妊娠和心脏病登记注册表(ROPAC)是一个全球性,前瞻性的结构性心脏病女性观察性登记,该登记注册提供了一个独特的大型研究人群。研究人员分析了中度(峰值梯度36至63mm Hg)和严重AS(峰值梯度≥64mmHg)女性的数据。在ROP
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#孕前#
0
#JACC#
34
#受孕#
23
#ACC#
28
#主动脉瓣#
38
#主动脉#
0
继续关注!
67
谢谢分享!
1