IBD: 克罗恩病患者术后早期生物治疗与较低的内镜复发率和长期结果改善相关
2022-07-11 xuyihan MedSci原创
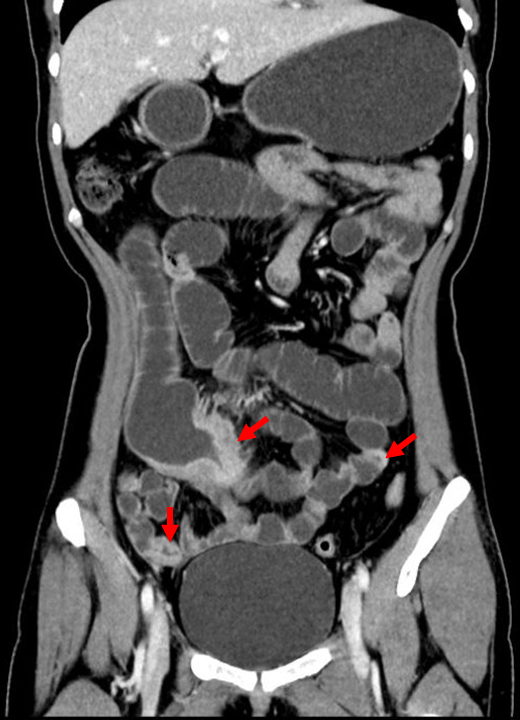
克罗恩病是一种原因不明的肠道炎症性疾病,在胃肠道的任何部位均可发生,但多发于末端回肠和右半结肠。本病和慢性非特异性溃疡性结肠炎两者统称为炎症性肠病(IBD)。
克罗恩病 (CD) 是一种慢性致残性炎症性疾病,具有复发和缓解反复交替的特点。抗肿瘤坏死因子 α (TNF-α)、维多珠单抗和优特克单抗等生物疗法的引入彻底改变了 CD 患者的管理,显着改善了他们的预后和生活质量。然而,由于多种并发症(即狭窄、脓肿、瘘管)和药物治疗失败的出现,三分之二的患者在其一生中需要接受了手术治疗。不幸的是,手术不能治愈,高达 90% 的患者在 3 年内会发生内窥镜疾病复发,多达 40% 的患者会在 10 年内再次接受手术。狭窄、瘘管、吸烟、既往肠道切除术(尤其是>50 cm)、发病年龄过早和肛周疾病与内镜下复发率增加有关。因此,如果存在这些风险因素,则在手术后立即开始生物治疗,以防止术后复发。到目前为止,还没有关于这些患者的长期结果的数据,并且不知道术后使用生物制剂治疗是否可能对降低复发风险产生影响。本研究的目的是探究术后生物治疗对CD患者内镜复发率和长期结果的影响。
这项回顾性队列研究于 2014 年至 2021 年在意大利米兰的几家中心医院进行。所有在术后 6-12个月接受手术和结肠镜检查的CD患者均符合入选条件。第一次的结肠镜检查被认为是基线水平,并且随着时间的推移对患者进行监测,以评估术后疾病的复发和长期疾病结果的发生。

研究最后共纳入141名患者(42.6% 为女性,平均年龄 44 岁)。中位随访时间为 28 个月。大约三分之一的患者在基线结肠镜检查时接受了生物制剂治疗。与接受治疗的患者相比,结肠镜检查时未接受生物治疗的患者的内镜复发率更高(80.8% vs 45.2%,P<. 0001)。未治疗患者的住院和手术发生率高于接受生物治疗的患者(12.1% vs 0.0%,P=. 01)。Kaplan-Meier 曲线显示,基线时未治疗组的5年住院率和手术率明显更高(23.3% VS49.7%,P =.0013) 。在逻辑回归模型中,缺乏生物治疗与内镜下疾病复发的风险独立相关(OR,0.22;95% CI,0.1-0.51;P = .0004 )。

本项研究结果表明,生物制剂治疗可能对所有患者术后均有益。接受生物治疗的患者内镜和组织学复发率降低。此外,生物治疗与降低长期负面结果的风险有关,包括手术、住院和药物治疗升级的需要。
原始出处:
Ferdinando D’Amico. Et al. Early Biological Therapy in Operated Crohn’s Disease Patients Is Associated With a Lower Rate of Endoscopic Recurrence and Improved Long-term Outcomes: A Single-center Experience. Inflammatory Bowel Diseases.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#长期结果#
38
#复发率#
42
学习了,谢谢分享
37
不错,学习了。
52
#内镜#
69
#IBD#
50