Lancet Haematol:金洁/主鸿鹄团队采用维奈克拉+DA方案治疗AML,首次CR高达91%
2022-05-03 MedSci原创 MedSci原创
急性髓细胞白血病(acute myelogenous leukemia, AML)是成年人最常见的急性白血病(约占80%以上),它的治疗仍以化疗为主,柔红霉素和阿糖胞苷组成的DA方案(也称&ldquo
急性髓细胞白血病(acute myelogenous leukemia, AML)是成年人最常见的急性白血病(约占80%以上),它的治疗仍以化疗为主,柔红霉素和阿糖胞苷组成的DA方案(也称“3+7”方案)是成人AML的标准诱导方案,该方案的一疗程缓解率在年轻AML患者(<60岁)中约为60%~65%,在老年AML患者中(≥60岁)约为40%~50%;5年生存率在年轻患者中仅为40~50%,在老年患者中<10%。但有70%左右获得缓解的患者最终复发并演变为难治性白血病,导致治疗失败而死亡。这套化疗方案持续了50年间,其地位没有重大变化。因此,如何在DA方案基础上,探索新的诱导治疗来进一步改善AML患者的预后是巨大的挑战。
浙江大学附属第一医院血液科金洁教授团队2000年初设计的HAA方案(国内多中心的临床研究中显示比国际标准方案缓解率提高了12个百分点,达到73%的CR率(Lancet Oncology 2013)。但是仍有近30%的AML患者无法获得CR,进一步提高这部分患者的CR率是临床的迫切需求。随着维奈克拉(Venetoclax)在国内上市,AML的治疗方案有望获得进一步突破。既往研究表明,维奈克拉联合阿扎胞苷或小剂量阿糖胞苷在老年AML患者中疗效明确(NEJM:维奈妥拉联合阿扎胞苷治疗老年急性髓系白血病)(Clin Cancer Res:维奈托克+阿扎胞苷可显著改善IDH1/2突变AML患者的预后)。因此,本研究旨在评估维奈克拉联合“3+7”方案(DAV方案)治疗成人初治AML患者的疗效和安全性。
这是一项研究者发起的、多中心、两阶段、2期临床试验。入组年龄为18~60岁且根据世界卫生组织(WHO)标准通过骨髓检查确诊为既往未经治疗的新发AML患者。纳入标准为患者ECOG评分为0~2分,接受DAV(柔红霉素 60mg/m2/d, qd,静脉注射,d1~d3;阿糖胞苷100mg/ m2/d, qd,静脉注射,d1~d7;维奈克拉 100mg d4, 200mg d5, 400mg d6~d11,qd,口服)作为诱导治疗方案。部分缓解且原始细胞下降60%或以上的患者给予第2疗程相同的诱导方案。诱导治疗1个疗程后不符合上述标准或诱导治疗2个疗程后未达到CR或CRi的患者退出研究,并使用其他挽救治疗方案重新诱导。缓解后治疗根据中国成人急性髓系白血病(非APL)诊治指南(2017)的预后风险进行分层治疗。该研究在www.chictr.org.cn上注册,注册号为ChiCTR2100045780。
主要终点为第一周期后复合缓解率(CRc:CR+CRi),次要终点包括通过流式细胞术检测的微小残留病灶(MRD)、无事件生存率(EFS)、总生存率(OS)和不良事件。
本研究自2020年12月25日至2021年7月7日期间,共招募了三家医院的36名成人新发AML患者,最终33名患者进入评估。15 名 (45%) 患者为男性,18 名 (55%) 为女性,均为亚洲人。 中位年龄40岁,细胞遗传学中高危患者占76%,ELN风险评估中高危患者占42%,患者人口统计学和基线特征如表1所示。
表1 患者基线特征
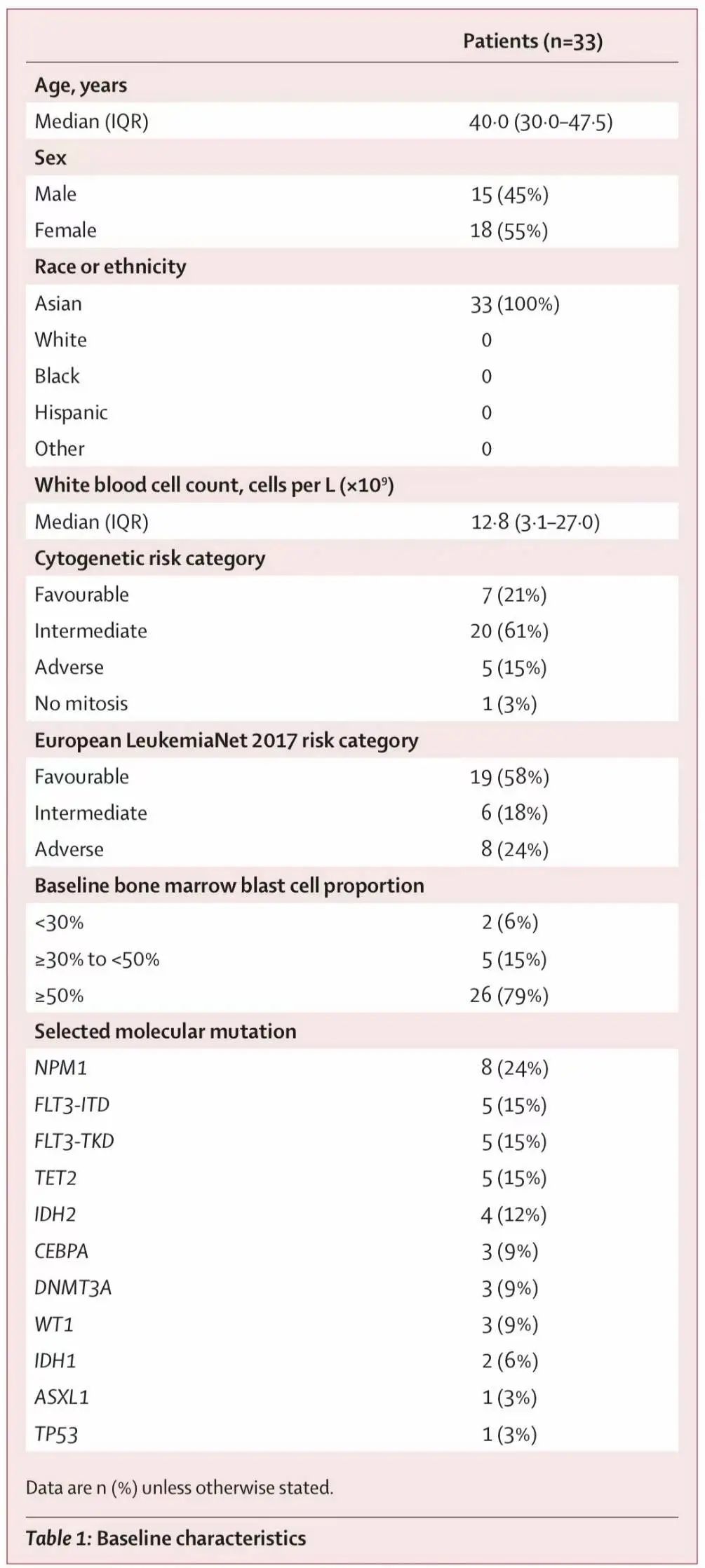
表2 治疗反应评估
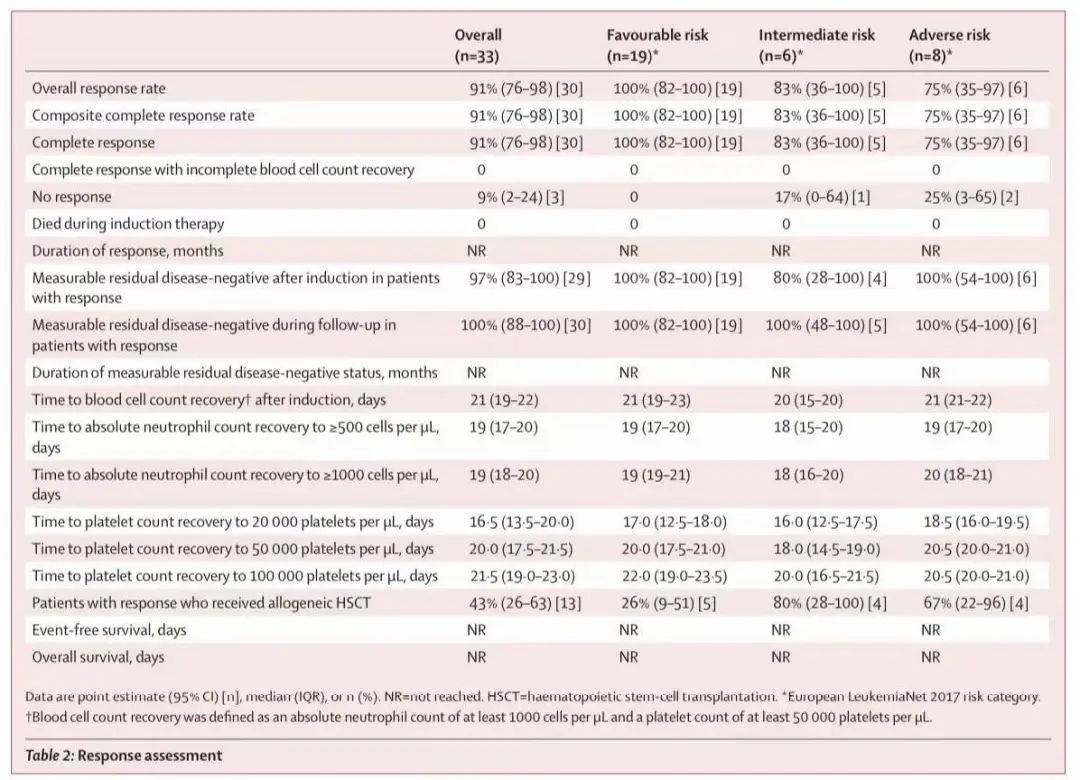
进一步分析不同分子亚型患者的结局。在7例RUNX1-RUNX1T1患者中,2例在DAV诱导治疗一个疗程后分子水平下降了3 log,4例达到完全分子学缓解(CMR)(<0.01%)。在8例NPM1突变患者中,7例达到CMR。在2例CBF-β-MYH11患者中,1例达到CMR,另1例分子水平下降了3 log。在3例MLL重排患者中,2例达到CMR,另1例在两个疗程后分子水平下降了3log。3例MLL重排患者随后均接受了异基因造血干细胞移植(allo-HSCT)。
中位随访 11 个月 (IQR 9-12),30例缓解患者中有4例复发(2例在完成所有要求的治疗方案后复发,2例在allo-HSCT后复发)。未达到中位OS、DFS和EFS时间,1年估计OS、DFS和EFS分别为96.8%(95%CI 90.8-100)、80.1%(95%CI 63.9-100)和72.1%(95%CI 55.6-93.5)。
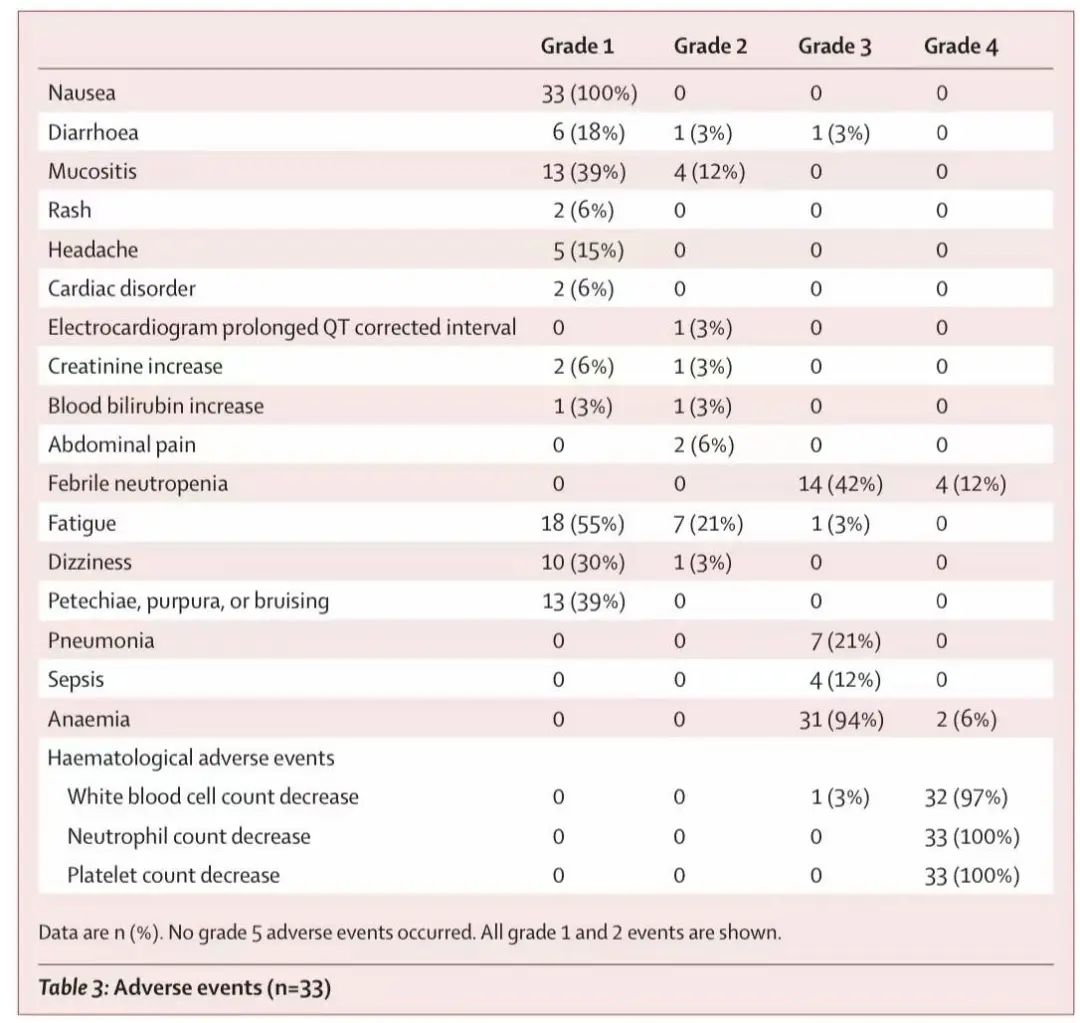
安全性分析显示,DAV第一个周期诱导治疗期间的不良事件(AE)如表3所示。未观察到5级AE。最常见的3~4级非血液学AE为发热性中性粒细胞减少(18例(55%)),肺炎(7例(21%))、脓毒症(4例(12%))、疲乏(1例(3%))和腹泻(1例(3%))。未观察到肿瘤溶解综合征。最常见的3~4级血液学毒性为中性粒细胞减少症(33例(100%))、血小板减少症(33例(100%))和贫血(33例(100%))。诱导治疗后缓解患者的血细胞恢复计数(中性粒细胞计数≥1000/μl;血小板计数≥50000/μl)的中位时间为21天(IQR 19-22天)。所有患者均未发现早期死亡,以及无治疗相关死亡。无患者需要调整剂量或因药物相关毒性而停药。
表3 不良事件汇总(n=33)
这项研究表明,在标准DA方案基础上添加维奈克拉组成的新的DAV方案,诱导治疗1个疗程后,可获得高达91%的CR率。并且DAV方案还与深度缓解相关,MRD阴性率高达97%,且与骨髓抑制快速恢复,诱导后恢复的中位时间为21天。此外,97%达到CR的患者保持MRD阴性状态直至末次随访。DAV方案的这种缓解深度也可能潜在改善AML患者的生存结局。因此DAV方案对新诊断的成人AML患者是一种有效的诱导治疗方案,可获得更高、更深缓解,且患者安全耐受性良好。本研究结果将为DAV方案在新诊断成人AML患者中的应用提供依据。
同时这项2期研究令人鼓舞的结果将由同一课题组正在进行中的比较新诊断成人AML患者DAV和DA方案的随机对照试验(ChiCTR2100045780)来进一步验证。
Huafeng Wang, Liping Mao, Min Yang, Pengxu Qian,Huan Lu,Hongyan Tong, Wanzhuo Xie, De Zhou, Xin Huang, Yungui Wang, Gaixiang Xu, Ying Lu, Juying Wei, Wenyuan Mai, Xiujin Ye, Haitao Meng, Yaojia Shen, Jian Huang, Wenjuan Yu, Jie Sun, Jianpeng Sheng, Xiaoyan Yan, Jie Jin†, Hong-Hu Zhu. Venetoclax plus“3+7”chemotherapy as the first-line therapy for adult patients with acute myeloid leukemia: a cohort from a multi-centre, singlearm, phase 2 trial. Lancet Haematol 2022. Published Online May 2, 2022
Homoharringtonine-based induction regimens for patients with de-novo acute myeloid leukaemia: a multicentre, open-label, randomised, controlled phase 3 trial.Lancet Oncol. 2013 Jun;14(7):599-608
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
44
#HAE#
39
学习了
66
#EMA#
46
学习了,等待进一步的结论
0
lancet上果然牛,感谢梅斯更新及时
30
认真学习~~
79