AJKD:在血液透析患者中应用telelcalcetide可降低甲状旁腺激素水平,减少相关并发症
2022-03-19 网络 网络
慢性肾脏疾病矿物质和骨骼疾病(CKD-MBD)以及继发性甲状旁腺功能亢进(SHPT)是需要透析的肾衰竭患者的常见并发症
慢性肾脏疾病矿物质和骨骼疾病(CKD-MBD)以及继发性甲状旁腺功能亢进(SHPT)是需要透析的肾衰竭患者的常见并发症。CKD-MBD主要表现为血清甲状旁腺激素(PTH)水平显著升高和血清钙磷水平异常调节,与多种不良心血管、骨骼和临床结果相关。
2003年KDOQI指南建议将PTH水平维持在150-300 pg/mL范围内。2009年,根据低水平证据,国际KDIGO临床实践指南建议将PTH目标值提高到正常上限(约130-585 pg/mL)的2到9倍,这导致美国许多血液透析(HD)设施的PTH目标值上限范围从300 pg/mL突然大幅改变。
伴随着PTH目标的增加,透析结果和实践模式研究(DOPPS)实践监测表明,在过去十年中,美国HD患者血清PTH水平高于600 pg/mL的比例从11%增加到23%。几项大型观察性研究一致表明,PTH高(≥600 pg/mL)的HD患者死亡率较高。
临床试验数据已经证明了端钙西肽(telelcalcetide)在降低血液透析(HD)患者甲状旁腺激素(PTH)水平方面的有效性。在本研究中,研究者提供了一份自2017年4月在美国推出以来的真实世界中端钙西肽的使用、剂量、有效性和停药总结。
美国透析结果和实践模式研究(DOPPS)显示,从2017年4月到2019年8月,在一项成人维持型HD患者的国家样本中有2596名新用户使用了telelcalcetide,研究者观察了钙肽起始后12个月的剂量轨迹,慢性肾病矿物质和骨病(CKD-MBD)药物,甲状旁腺激素(PTH)水平,血清钙和磷水平。
研究结果显示,从2017年4月首次使用依替卡西肽开始到2019年8月,依替卡西肽处方在HD患者中增加到6%。70%的患者开始服用依替卡西肽的剂量为15 mg/wk,27%的患者为7.5 mg/wk,49%的新用户在前3个月内服用了依替卡西肽。在起效后3个月、6个月和12个月,依替卡西肽停药率分别为9%、17%和27%。
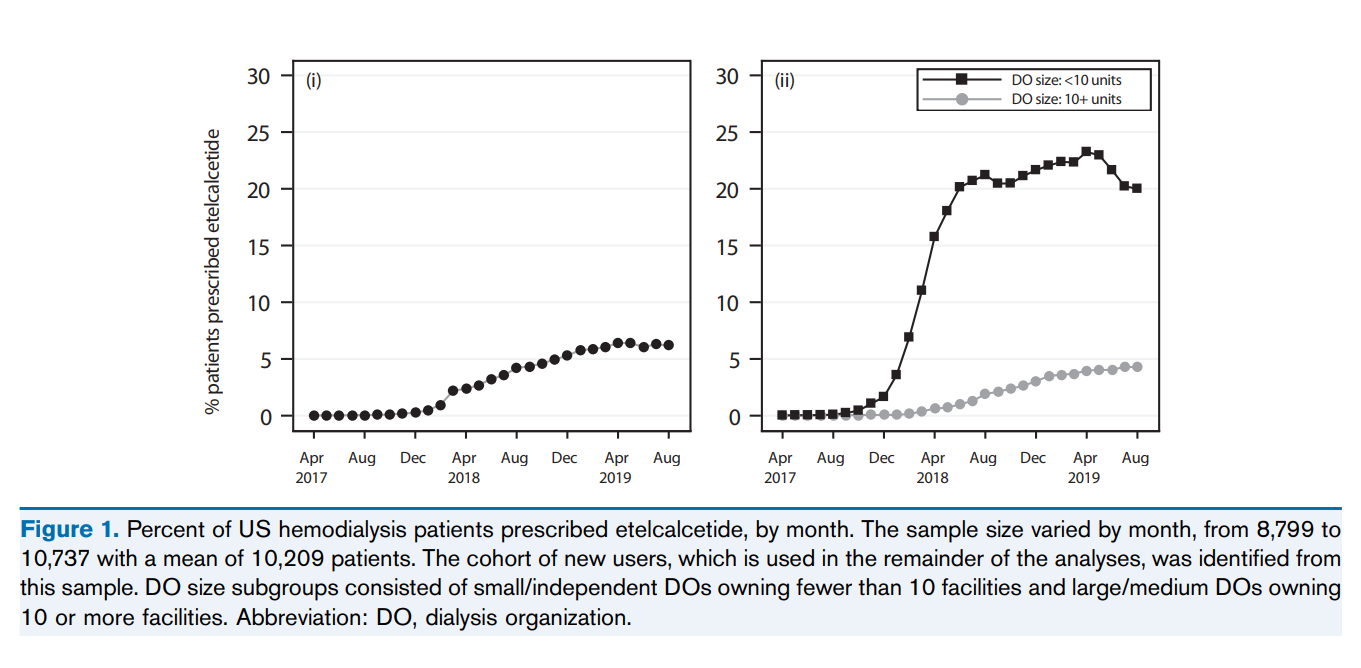
美国血液透析患者按月开用依替卡西肽的百分比
在依替卡西肽开始使用一年后,平均PTH水平下降了40%,从948 pg/mL降至566 pg/mL,PTH在目标范围内(150-599 pg/mL)的患者比例总体上从33%上升到64%,在基线PTH 600 pg/mL的患者中从0%上升到60%,在之前使用过伊特卡西肽的患者中从30%上升到63%。
血清磷>5.5 mg/dL的患者比例从55%降至45%,而白蛋白校正血清钙<7.5 mg/dL的患病率保持在1%-2%。在依替卡西肽开始使用后的12个月内,活性维生素D(从77%增加到87%)和钙基磷酸盐粘合剂(从41%增加到50%)的使用有所增加。
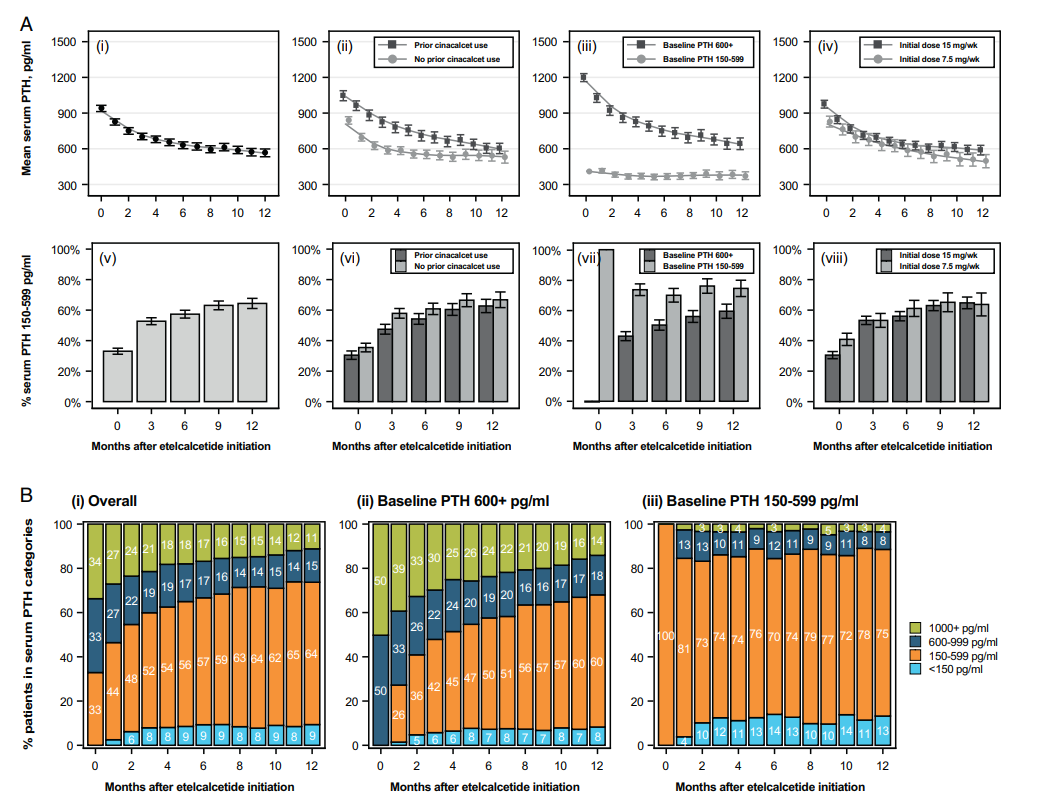
血清甲状旁腺激素(PTH)平均值和目标甲状旁腺激素(PTH)范围(150-599 pg/mL)的变化轨迹
总之,本研究结果显示,在依替卡西肽启动后的12个月,患者的甲状旁腺激素水平大幅持续下降。这些结果支持使用依替卡西肽作为一种有效的治疗方法,以实现KDOQI推荐用于HD患者CKD-MBD的指南。
参考文献:Angelo Karaboyas, Daniel Muenz, Douglas S. Fuller, et al. Etelcalcetide Utilization, Dosing Titration, and Chronic Kidney Disease–Mineral and Bone Disease (CKD-MBD) Marker Responses in US Hemodialysis Patients, American Journal of Kidney Diseases, Volume 79, Issue 3, 2022, Pages 362-373, ISSN 0272-6386, https://doi.org/10.1053/j.ajkd.2021.05.020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#激素水平#
41
#相关并发症#
38
#并发#
36
#血液透析#
50
#甲状旁腺#
40
#透析患者#
47