J Natl Cancer Inst:可对HPV相关性口咽癌进行风险分层的肿瘤浸润淋巴细胞影像学标记物!
2021-12-09 Nebula MedSci原创
可对HPV相关性口咽癌进行风险分层的肿瘤浸润淋巴细胞影像学标记物。
与非病毒相关的口咽鳞状细胞癌 (OPCSCC) 相比,HPV相关性口咽鳞状细胞癌有极好的控制率。多项试验正在积极测试,降低这些患者的治疗强度是否能在减少治疗相关毒性的同时维持肿瘤平衡。
Corredor等研究人员开发了一种生物标记物 OP-TIL,可在组织学图像中表征肿瘤浸润淋巴细胞 (TIL) 和周围细胞之间的空间相互作用。本研究探究了OP-TIL是否可将I期的HPV相关性OPSCC患者进一步分成低风险组和高风险组,并帮助患者选择降级临床试验。
采用来自6个机构队列的439位I期的HPV相关性OPSCC患者的H&E切片分析IP-TIL和患者预后的相关性。然后采用另一队列研究(n=94)明确最具预后意义的特征,训练Cox回顾模型以预测复发和死亡风险。最后采用生存性分析在其余5项队列(n=345)中验证该算法作为复发/死亡生物标志物的准确性。
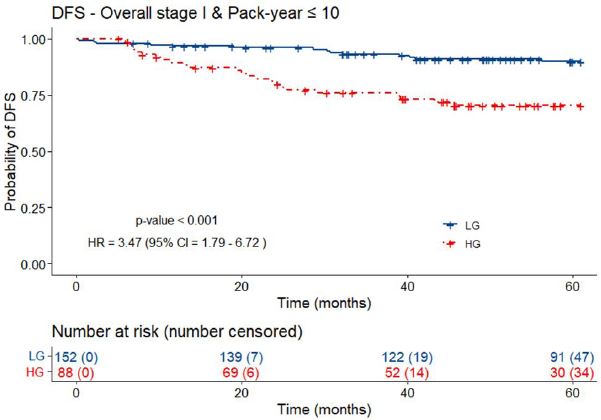
有≤10包/年吸烟史的低风险组和高风险组患者的DFS
OP-TIL将有≤30包/年吸烟史的I期HPV相关性OPSCC患者分成了低风险组(2年无病生存率[DFS] 94.2%;5年DFS 88.4%)和高风险组(2年DFS 82.5%;5年DFS 74.2%;风险比 2.56,p<0.001);在DFS的多变量分析中,即使根据年龄、吸烟状态、T和N分类、以及治疗方案进行校正后,上述相关性仍然存在(风险比 2.27,p=0.003)。
有≤30包/年吸烟史的低风险组和高风险组患者的DFS
综上,OP-TIL可以筛选出或可进行降级治疗的低风险的I期HPV相关OPSCC患者。OP-TIL有望成为一种生物标志物,以用于临床优化患者的降级选择。
原始出处:
Corredor Germán,Toro Paula,Koyuncu Can et al. An Imaging Biomarker of Tumor-Infiltrating Lymphocytes to Risk-Stratify Patients with HPV-Associated Oropharyngeal Cancer.[J] .J Natl Cancer Inst, 2021, https://doi.org/10.1093/jnci/djab215.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
42
#NST#
46
#标记物#
48
#ATL#
0
#相关性#
31
#淋巴细胞#
33
#口咽癌#
0
#风险分层#
52