生物制剂CD24Fc治疗重症COVID-19:III期临床取得积极进展
2020-06-15 Allan MedSci原创
OncoImmune制药公司近日公布,其实验性生物制剂CD24Fc治疗重症COVID-19患者的III期临床证明了CD24Fc的安全性和有效性。
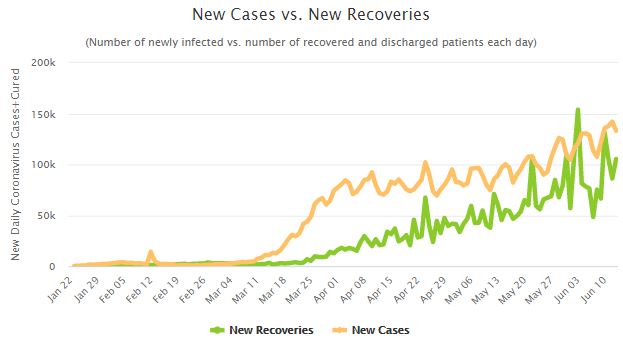
OncoImmune制药公司近日公布,其实验性生物制剂CD24Fc治疗重症COVID-19患者的III期临床证明了CD24Fc的安全性和有效性。当前COVID-19的治疗策略包括使用阻断病毒复制的抗病毒疗法和针对宿主反应的非抗病毒疗法。由于许多住院患者要么已经很大程度上清除了SARS-CoV-2病毒,要么已经出现针对病毒的免疫力,因此非抗病毒策略已成为治疗重症COVID-19患者的重要方法。
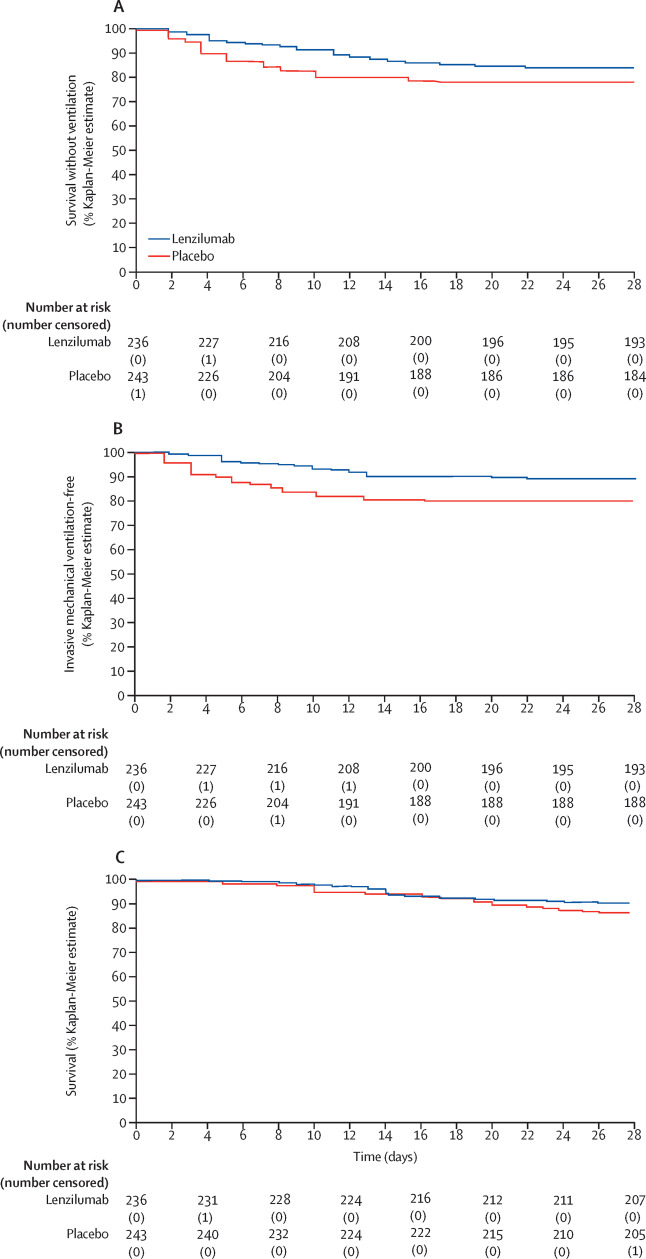
CD24Fc可防止由组织损伤引起的过度炎症。III期试验已招募了230例需要补充氧气的重症COVID-19患者。在试验开始时,患者接受CD24Fc或安慰剂的单次输注,之后随访28天,以确定从重症到轻症的时间(主要终点)。由于该药物通过一种新颖的机制起作用,且该机制与其他实验性疗法没有重复,因此无需排除参加过其他试验的患者。

原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#生物制剂#
31
#III#
25
#I期临床#
23
#II期临床#
0
#III期#
30