肺动脉高压所致右心室衰竭的蛋白质组学和代谢组学分析
2022-07-24 刘少飞 MedSci原创
该研究描述了MCT诱导的PAH进展过程中RV心肌的蛋白质组和代谢组概况,同时也为潜在的治疗目标提供了见解,促进了PAH中RV功能障碍的延缓或逆转。
右心室衰竭(RVF)是肺动脉高压(PAH)死亡的独立和最有力的预测因素,但是,目前还没有直接针对衰竭的右心室(RV)的预防和治疗策略。RV肥大(RVH)和功能障碍的基本机制需要深入探讨。在这项研究中,我们利用心肌蛋白质组学与代谢组学相结合的方法,阐明了野百合碱(MCT)诱导的PAH大鼠模型中RV重塑的潜在病理生理学变化。使用无标签液相色谱-串联质谱法(LC-MS/MS)鉴定了从RV心肌中提取的蛋白质和代谢物。生物信息学分析表明,细胞内Ca2+浓度的升高和炎症可能有助于心肌的增殖和收缩,这可能有利于维持RV的代偿状态。在RVF阶段,铁萎缩、线粒体代谢转变和胰岛素抵抗都明显参与。铁平衡失调、谷胱甘肽代谢和脂质过氧化与铁质沉着有关,可能会导致房车失调。总之,我们描述了MCT诱导的PAH进展过程中RV心肌的蛋白质组和代谢组概况,同时也为潜在的治疗目标提供了见解,促进了PAH中RV功能障碍的延缓或逆转。
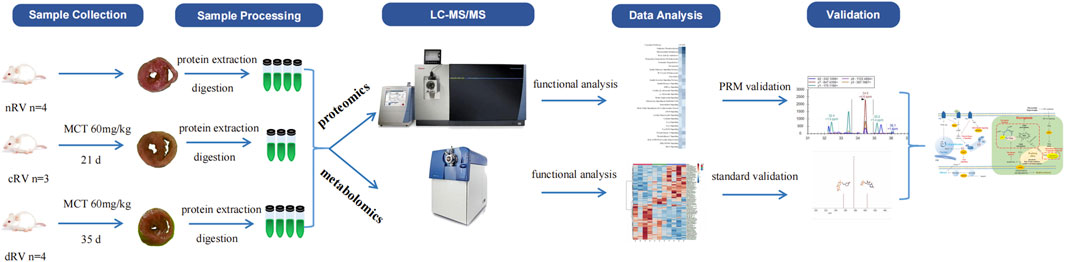
在这项研究中,我们分析了RV心肌的蛋白质组和代谢组,确定了DEP,以及与nRV相比,cRV和dRV的代谢物的改变,这加深了我们对MCT诱导的PAH大鼠模型中RV适应和衰竭变化的理解。它可能为机制探索提供线索,并促进治疗的进展。根据功能注释,我们建立了一个模式,描述了通过RVF进展在分子和通路水平上的主要推断变化(图2)。
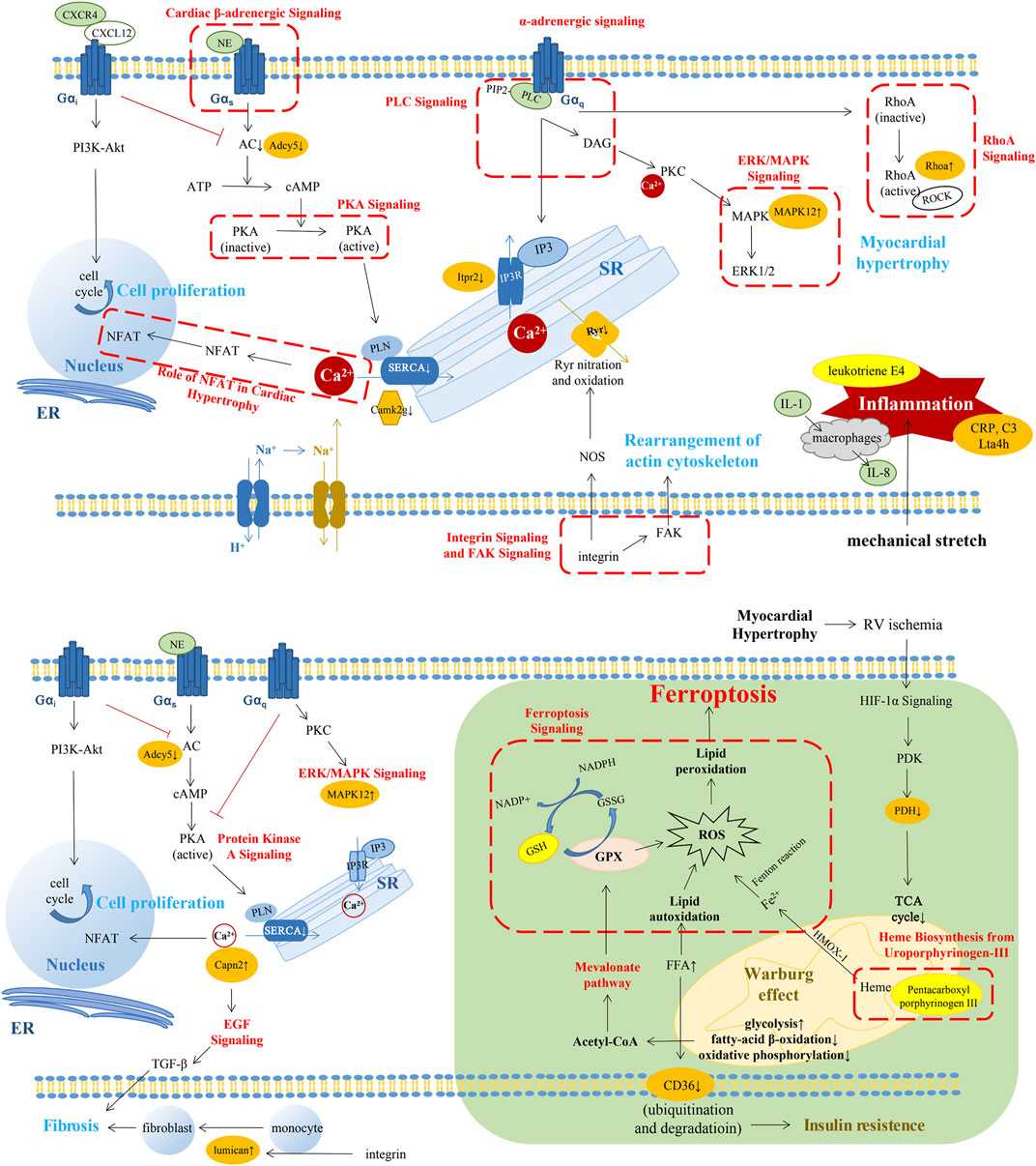
图2. 描述RVF发展过程中分子和通路水平的关键变化的总结模式。RV代偿阶段的变化(上)。RV失代偿期的变化(下图)。绿色背景的变化代表我们的新发现。红色字体或红色虚线框内的路径是与以前的研究相同的改变的路径。橙色亮点的分子代表了我们结果中重要的改变的蛋白质。带有亮黄色亮点的分子代表了我们研究结果中重要的代谢物的改变。SERCA2,肌质网(SR)Ca2+-ATP酶;PIP2,磷脂酰肌醇-4,5,-二磷酸;IP3,肌醇-1,4,5-三磷酸;Itpr2,肌醇1,4,5-三磷酸受体类型2。Camk2g,钙/钙调蛋白依赖性蛋白激酶II型亚单位γ;ADCY5,腺苷酸环化酶5型;MAPK,丝裂原激活蛋白激酶。DAG,二酰基甘油;NOS,一氧化氮合成酶;NFAT,活化T细胞的核因子;ROCK,RhoA-Rho激酶;Lta4h,白三烯A-4水解酶;GPX4,谷胱甘肽过氧化物酶4;HIF-1α,缺氧诱导因子1α;PDK,丙酮酸脱氢酶激酶;PDH,丙酮酸脱氢酶;FFA,自由脂肪酸。
总之,我们的研究提出了一个全面的RV蛋白质组和代谢组的概况,描述了PAH的疾病进展和伴随的RVF。在代偿阶段,神经荷尔蒙激活、Ca2+平衡和炎症可能导致RVH而保留RV功能。在失代偿阶段,线粒体功能障碍、胰岛素抵抗和脂肪毒性可能在dRV阶段相互关联,针对心肌代谢的治疗可能是一种有希望的方法。此外,铁中毒与PAH以及RV功能之间的具体关系仍有待于进一步挖掘。如果代谢干预、二甲双胍的治疗效果和抑制铁蛋白酶的作用能够延缓房室功能的恶化,则需要在更高的循证研究中得到进一步验证。
对于未来的研究前景,以下几个方面可以进一步改进。首先,本研究的样本量相对较小,更多的样本将用于验证本研究的结果。第二,我们使用的是MCT诱导的大鼠模型,这是一个单一的病理损伤模型,而MCT可能对心肌和其他器官有一定的毒性。因此,我们的研究结果应在其他PAH动物模型、相关细胞系和临床样本中得到验证。第三,我们的研究集中在代偿期和失代偿期之间与对照期的变化。在代偿期和失代偿期之间是否还有我们没有发现的其他途径,需要进一步研究。第四,我们的研究是一个试验性的omics研究,该疾病的具体机制途径需要更多的基础研究的功能实验来支撑。
参考文献:
Qin X, Lei C, Yan L, Sun H, Liu X, Guo Z, Sun W, Guo X, Fang Q. Proteomic and Metabolomic Analyses of Right Ventricular Failure due to Pulmonary Arterial Hypertension. Front Mol Biosci. 2022 Jul 5;9:834179. doi: 10.3389/fmolb.2022.834179. PMID: 35865003; PMCID: PMC9294162.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉高压#
46
#白质#
40
#代谢组#
50
#蛋白质组#
47
#蛋白质#
61
#代谢组#
44
#右心室#
50