AJRCCM:Y染色体基因Uty通过减少促炎症化合因子保护肺动脉高压
2022-07-23 刘少飞 MedSci原创
根据以前发现,Y染色体对缺氧诱导的实验性肺动脉高压(PH)有保护作用,这可能有助于PAH的性别差异。在此,我们确定了Y染色体的保护基因,研究了关键的下游常染色体基因,并展示了一种新的临床前疗法。
研究背景:
特发性肺动脉高压(PAH)是一种以肺动脉压力增加、右心室衰竭和死亡为特征的恶性的肺血管疾病。PAH表现为显著的性别偏向,女性的发病率高于男性了解性别差异背后的分子基础可能有助于发现新的治疗方法。
研究目的:
根据以前发现,Y染色体对缺氧诱导的实验性肺动脉高压(PH)有保护作用,这可能有助于PAH的性别差异。在此,我们确定了Y染色体的保护基因,研究了关键的下游常染色体基因,并展示了一种新的临床前疗法。
研究主要结果:
敲除Y染色体基因Uty导致更严重的PH,其衡量标准是右心室压力增加和肺动脉加速时间减少。RNA测序显示,由于Uty被敲除,促炎症趋化因子Cxcl9和Cxcl10增加。该研究发现CXCL9和CXCL10在人类PAH肺部明显上调,在女性PAH患者中上调更为强烈。用CXCL9和CXCL10处理人肺动脉内皮细胞会引发细胞凋亡。抑制雄性Uty基因敲除小鼠的Cxcl9和Cxcl10的表达以及抑制雌性大鼠的CXCL9和CXCL10的活性可显著降低PH的严重程度。
研究结论:
Uty对PH有保护作用。减少Uty的表达会导致促炎症趋化因子Cxcl9和Cxcl10的表达增加,从而引发内皮细胞死亡和PH。抑制CLXC9和CXLC10可以逆转多个PH实验模型的疾病进展。
该研究回答了什么科学问题?
特发性肺动脉高压(IPAH)是一种恶性的肺血管疾病,它显示出明显的性别差异,尤其女性受到严重的影响。
几十年来,人们一直在研究这种性别差异性的根本原因,重点一直是研究性激素的作用。然而,该研究团队的实验室是第一个研究性染色体在PAH方面的潜在作用的实验室。本研究发现男性特异性Y染色体对实验性肺动脉高压(PH)有保护作用,它确定了Y染色体基因Uty通过抑制肺部的促炎症途径来保护男性免受PAH的发展。当Uty在男性中低表达或在女性中不表达时,趋化因子Cxcl9和Cxcl10的表达增加,导致血管内皮细胞功能紊乱和更严重的PH发展。我们还证明,在两个临床前大鼠模型中,针对这一下游炎症途径足以降低PH的严重程度。
研究细节:
图1. 肺部特异性敲除Uty,而不是其他在肺部表达的Y染色体(ChrY)基因,消除了ChrY对缺氧(Hx)引起的肺动脉高压的保护。

该课题组在2018年发现,Y染色体对缺氧引起的小鼠PH具有保护作用(Am J Respir Crit Care Med.2018 Apr 1; 197(7): 952–955.),本研究在此基础上发现只有四个编码蛋白质的ChrY基因在小鼠肺组织中表达,即Ddx3y(Y型连接的DEAD-box螺旋酶3)、Eif2s3y(真核翻译起始因子2,亚单位3,结构基因Y型连接)、Kdm5d(赖氨酸脱甲基酶5D)和Uty。这其中的三个,Ddx3y、Kdm5d和Uty在人类中是保守的,与健康病人的肺相比,KDM5D和UTY在男性PAH病人的肺中都被发现是下调的。
图2. 促炎性趋化因子CXCL9和CXCL10是Uty下游的常染色体阻断剂,在PAH患者肺部以性别特异性方式上调。
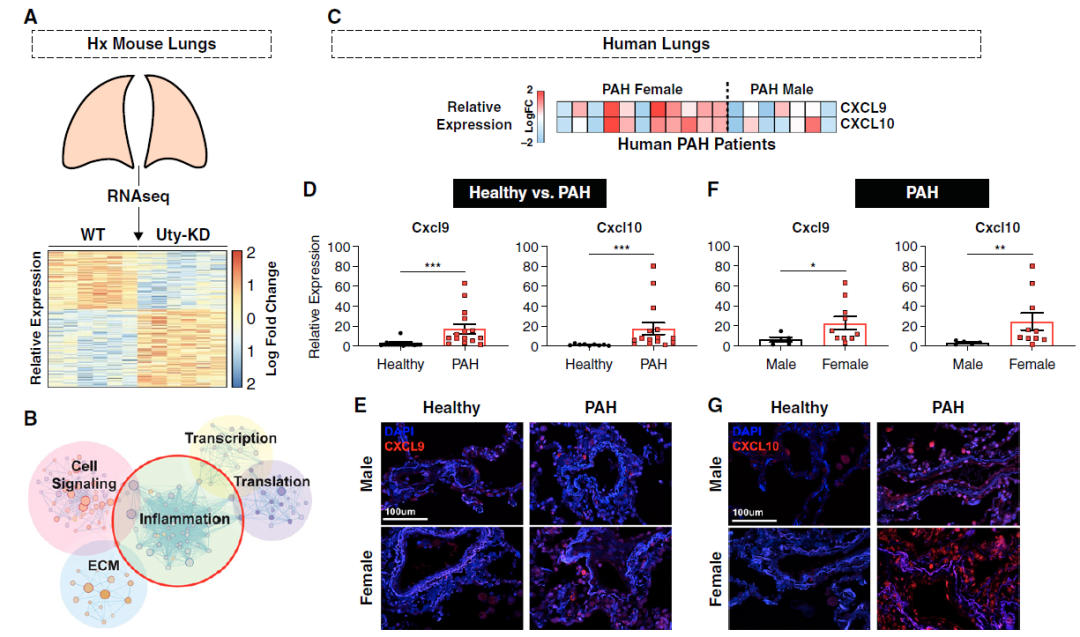
为了揭示Uty在PH中保护的分子机制,该研究对Hx Si-Scrm和Si-Uty小鼠肺组织进行了RNA测序,确定了523个DEGs(图2A)。信号通路富集分析突出了五个主要的通路,其中炎症尤其富集(图2B)。由于炎症在PAH的发病机制和严重程度上起着主要作用,研究把重点放在炎症性DEGs上。随后,炎症性DEG集与PAH患者肺组织的在线芯片进行交叉比对,并搜索在Si -Uty(与Si -Scrm相比)和女性PAH样本(与男性样本相比)中都升高的基因。这项分析产生了两个最感兴趣的基因:促炎症趋化因子CXCL9和CXCL10(图2C),通过验证了这两个基因在男性和女性PAH肺部与健康肺部相比都是上调的,与男性患者相比,女性PAH患者的上调更为强劲(图2D和2F)。这些数据由人类健康和PAH肺部的免疫荧光图像表示(图2E和2G)。
图3. 全身的Uty-KO促进了更严重的PH进展,而这一表型可被Cxcl9和Cxcl10的Knock-Down所阻止。

由于肺部特异性Uty-KD导致PH严重程度增加,Cxcl9和Cxcl10表达升高,该研究进一步深入了解1)全身Uty-KO小鼠是否也发展出更严重的PH;2)敲除Uty-KO小鼠的Cxcl9和Cxcl10是否足以降低PH严重程度(图3A)。研究发现,与GDXWT雄性小鼠相比,暴露于慢性Hx的GDX Uty-KO雄性小鼠表现出RVSP升高,PAAT和PAAT/RVET比率降低(图3B和3C)。与完整的Hx WT雄性相比,在性腺完整的Hx Uty-KO动物中也观察到更严重的PH,尽管性腺激素和PH严重性之间没有明显的相互作用。在Hx GDX Uty-KO小鼠的肺部联合KD Cxcl9和Cxcl10,导致RVSP和RV肥大明显减少,同时与Uty-KO对照组相比,PAAT和PAAT/RVET比率明显增加(图3B-3D)。同时验证了与接受非靶向性Si-Scrm的Uty-KO小鼠相比,接受靶向性siRNA的Uty-KO小鼠的肺部Cxcl9和Cxcl10表达明显减少(图3E)。
总的来说,与WT小鼠相比,Uty-KO小鼠在暴露于Hx时表现出更差的PH严重程度。肺部特异性KDof Cxcl9和Cxcl10足以减轻GDX Uty-KO小鼠的PH发展。
图4. Uty、Cxcl9和Cxcl10在巨噬细胞中共存,Uty表达与Cxcl9和Cxcl10表达成反比。
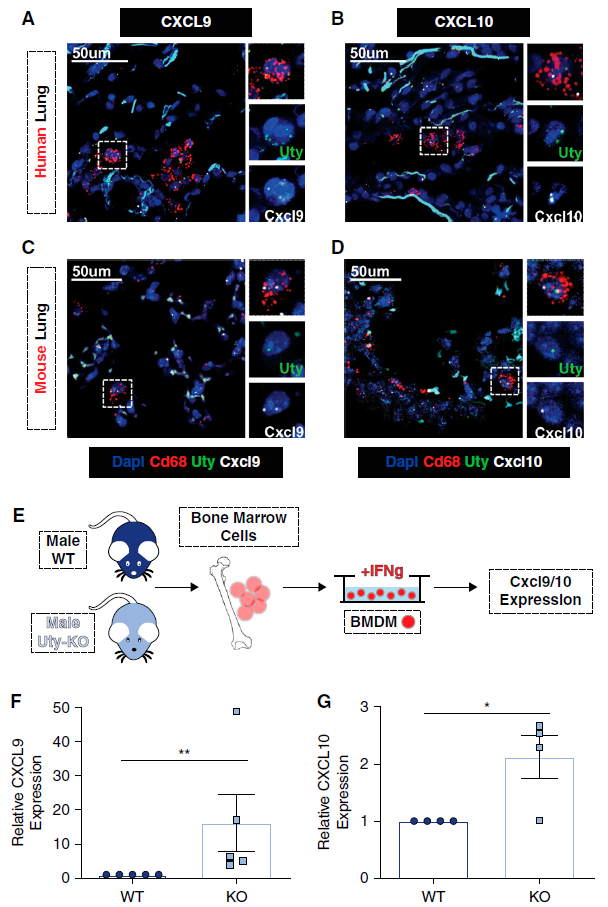
鉴于巨噬细胞在PH病理中越来越重要以及巨噬细胞表达CXCL9和CXCL10,该研究测试了Uty在肺部巨噬细胞中的表达。来自小鼠和人类肺部的染色组织切片证实了Uty在雄性组织的Cd681巨噬细胞中的表达,但在雌性组织中没有表达。尽管我们发现Uty与趋化因子Cxcl9和Cxcl10成反比,但我们发现了肺组织在巨噬细胞内的共聚焦情况,发现Uty转录本与Cxcl9(图4A和4C)和Cxcl10(图4B和4D)共聚焦。为了确定Uty在巨噬细胞中的表达是否直接影响Cxcl9和Cxcl10的产生,同时测量了BMDM中Cxcl9和 Cxcl9和Cxcl10在雄性WT和Uty-KOmice的BMDMs中的表达(图4E)。与WT小鼠相比,Uty-KO小鼠的BMDMs表达的Cxcl9和Cxcl10明显增多(图4F和4G)。UTY是Jumonji组织蛋白去甲基化酶家族的成员,但其作为H3K27去甲基化酶的作用在文献中存在很大争议。本研究考虑Uty在肺部的作用是否是通过去甲基化介导的,发现Uty在全肺和分离的肺巨噬细胞中的表达并不影响通过Western blot测量的H3K27三甲基化蛋白的水平。
总之,我们发现在肺部巨噬细胞中与Cxcl9和Cxcl10共定位的Uty调节Cxcl9和Cxcl10的表达,但对H3K27去甲基化没有明显影响。
图5. CXCL9和CXCL10重组蛋白引发肺动脉内皮细胞(PAEC)功能紊乱。
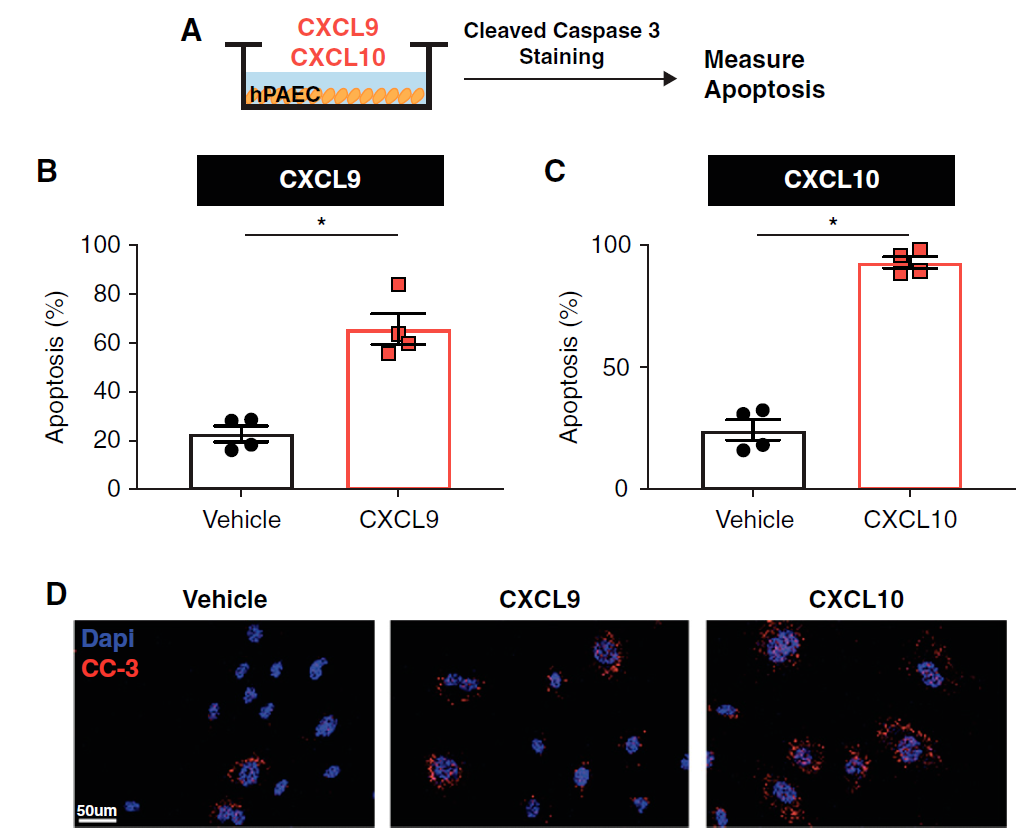
为了确定Uty下游常染色体基因Cxcl9和Cxcl10促进PH严重性的机制,该研究使用人类PAECs进行了体外细胞研究。PAECs表达共同的CXCL9和CXCL10受体CXCR3;PAEC功能障碍是PAH病症的一个标志,已知会通过血管生成失调、血管活性物质的分泌改变和血管通透性增加PH的严重程度。血管活性物质的分泌改变和血管通透性的增加。本研究将人PAECs与重组人CXCL9和CXCL10 蛋白,并测量其对EC功能障碍的影响(图5A)。用CXCL9或CXCL10处理PAECs导致PAEC凋亡的增加,通过定量测定裂解的 caspase-3染色(图5B-5D)。
图6. 在两个大鼠PH模型中,阻断CXCL9和CXCL10的活性足以逆转PH。
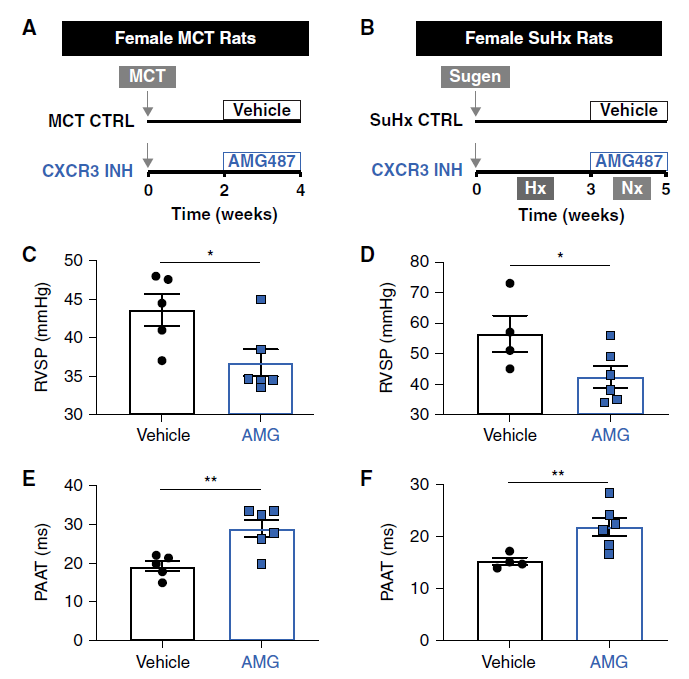

研究数据表明,Uty通过下调Cxcl9和Cxcl10的表达来提供PH保护(图3),而CXCL9和CXCL10则促进PAEC的功能障碍(图5)。CXCL9和CXCL10促进PAEC的功能障碍(图5)。因为该研究发现这些促炎症的趋化因子在人类PAH患者的肺部升高,在女性PAH患者中尤其高(图2),该研究测试了我们是否可以通过使用针对CXCR3的小分子抑制剂(AMG487)阻断CXCL9和CXCL10的活性,将Uty保护的主题扩展到女性PH患者(图6A和6B)。为了更好地检查保护作用,该研究使用了大鼠PH的两个临床前模型,即MCT和SuHx模型,它们比小鼠的Hx更严重。该研究在雌鼠身上测试了我们的临床前治疗策略,以确定针对CXCL9和CXCL10是否是一种可行的PAH治疗策略。我们发现,AMG487充分拯救了MCT和SuHx模型中的PH发展,因为在PH刺激2或3周后用AMG487治疗的大鼠表现出明显较低的RV压力,同时PAAT、PAAT/RVET比值和RV分数面积变化增加(图6C-6F)。此外,在MCT模型中,AMG487处理的大鼠的房室肥大明显减少,而在SuHx模型中,RV肥大有减少的趋势(图6G-6H)。由于CXCL9和CXCL10在体外诱导PAEC凋亡,该研究旨在确定这种细胞机制是否有助于AMG487治疗赋予大鼠的PH保护。研究发现在接受治疗的MCT和SuHx大鼠的肺部,EC的凋亡减少了,这表明阻断CXCL9和CXCL10的作用减少了肺血管EC功能障碍(图6I-6L)。
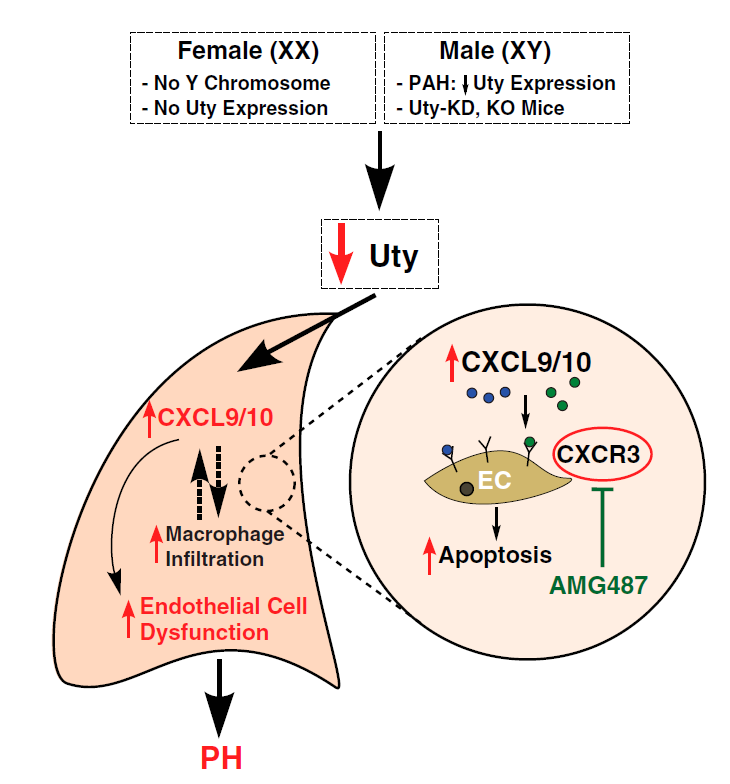
图7. Uty/Cxcl9/Cxcl10轴在PH发病机制中的拟议机制。Uty缺失(在雌性)或表达减少(在雄性PAH患者或Uty-KD或KO小鼠中)导致肺部促炎症趋化因子Cxcl9和Cxcl10的上调。
综上所述,我们的研究结果表明,在两种PH实验模型中,抑制共有的CXCL9和CXCL10受体是一种可行的临床前治疗策略,因为它可以减少PH的严重程度和肺血管EC功能障碍。
参考文献:
1. Umar S, Cunningham CM, Itoh Y, Moazeni S, Vaillancourt M, Sarji S, Centala A, Arnold AP, Eghbali M. The Y Chromosome Plays a Protective Role in Experimental Hypoxic Pulmonary Hypertension. Am J Respir Crit Care Med. 2018 Apr 1;197(7):952-955. doi: 10.1164/rccm.201707-1345LE. PMID: 28934553; PMCID: PMC6020406.
2. Cunningham CM, Li M, Ruffenach G, Doshi M, Aryan L, Hong J, Park J, Hrncir H, Medzikovic L, Umar S, Arnold AP, Eghbali M. Y-Chromosome Gene, Uty, Protects Against Pulmonary Hypertension by Reducing Proinflammatory Chemokines. Am J Respir Crit Care Med. 2022 Jul 15;206(2):186-196. doi: 10.1164/rccm.202110-2309OC. PMID: 35504005.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#促炎#
59
#动脉高压#
38
#RCC#
44
#染色体#
51
#Y染色体#
52
学习了,谢谢分享
0