Cancer Cell:乳腺癌转移未来或可阻断
2015-03-20 霍瑶 南方都市报
乳腺癌扩散转移是患者的噩梦,有没有一种药物,可以控制癌细胞的转移通道?中大孙逸仙纪念医院的研究人员往前迈了一步。3月9日,一篇发现调控乳腺癌转移新机制的论文,登上国际肿瘤学最高学术期刊之一《癌细胞》(Cancer Cell)。人话版 • 肿瘤内部的炎症因子可以激活NFκB,打开通路让癌细胞转移。 • 不过要激
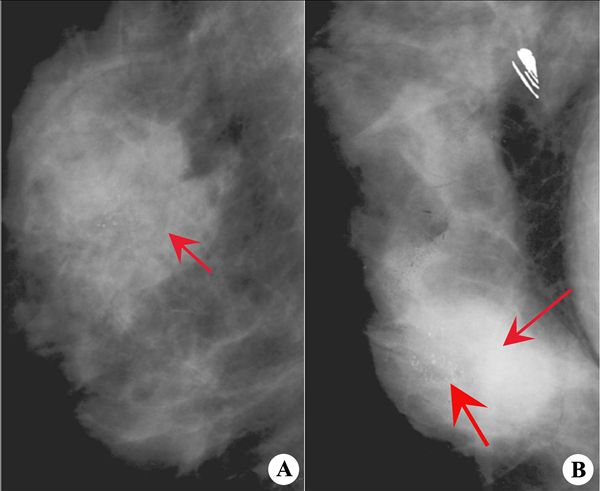
乳腺癌扩散转移是患者的噩梦,有没有一种药物,可以控制癌细胞的转移通道?中大孙逸仙纪念医院的研究人员往前迈了一步。3月9日,一篇发现调控乳腺癌转移新机制的论文,登上国际肿瘤学最高学术期刊之一《癌细胞》(Cancer Cell)。这篇研究发现长链非编码RNA (lncRNA)中能与重要的炎性转录因子NF-κB相作用的NKILA,控制了肿瘤的炎性信号,通过阻断肿瘤的炎性信号,将来有望肿瘤肿瘤的转移的可能。这一研究也为炎-癌互作提供重要的理论基础。
人话版
- 肿瘤内部的炎症因子可以激活NFκB,打开通路让癌细胞转移。
- 不过要激活NFκB这条通道,就要干掉IκB这个守门员。这个守门员很弱,就像希腊神话中阿喀琉斯之踵,肿瘤微环境很容易把它灭掉。
- 一条非编码RNA被发现可以保护IκB,就像给阿喀琉斯穿了保护靴。这双靴子的牌子叫“NKILA”。是中大宋尔卫研究团队的功劳。
- 未来或许可以改装这双靴子,研发出抗癌药物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
25
#Cell#
35
中国学者
107
#阻断#
39
#cancer cell#
38
卢海的
142
#癌转移#
31
有点夸张,不过成果发表不错
116