CGH:37项临床试验的数据分析表明,使用DAA治疗HCV感染与VZV再激活风险增加之间无关联
2021-09-14 从医路漫漫 MedSci原创
接受直接抗病毒治疗(DAA)的丙型肝炎病毒(HCV)感染患者发生水痘-带状疱疹病毒感染(VZV再激活)的风险增加。
背景与目的:最近的病例和回顾性研究引起了人们的关注,即接受直接抗病毒治疗(DAA)的丙型肝炎病毒(HCV)感染患者发生水痘-带状疱疹病毒感染(VZV再激活)的风险增加。我们通过分析37个DAA药物临床试验的参与者数据,研究了DAA治疗与VZV再激活之间的关系。
方法:我们获得了37个临床试验的13816名参与者的人口学、不良事件和实验室数据,这些临床试验提交给美国食品和药物管理局批准DAA药物治疗HCV感染。参与者分别接受DAAs (n=12,249)、安慰剂(n=997)、聚乙二醇化干扰素(n=243)或DAAs和聚乙二醇化干扰素联合治疗(n=327)。VZV再激活的发生是根据系统报告的不良事件数据确定的。通过测量HCV RNA来评估HCV病毒学应答情况。
结果:在DAA治疗中,每1000人年有9.9例VZV再激活(95% CI, 6.8 - 14.0 / 1000人年)。在安慰剂组中,每1000人年有13.8例VZV再激活(95% CI, 3.5-37.5 / 1000人年),而聚乙二醇干扰素组或DAA和聚乙二醇干扰素联合组中没有VZV再激活。DAA治疗和安慰剂组之间的VZV再激活没有显著差异。VZV再激活与年龄大于40岁、女性和合并HIV感染相关。我们没有发现病毒学应答时间和VZV再激活时间之间具有关联性。
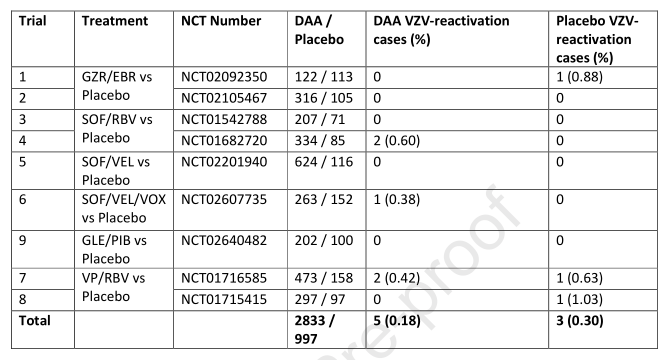
表 与安慰剂对照组的9个试验子集的vzv再激活率;除了试验4(包括240名接受24周DAA治疗的试验参与者)外,该子集的试验使用12周的治疗时间。DAA:直接的抗病毒药物;VZV:水痘一带状疱疹病毒。
结论:在对37项试验数据的分析中,我们没有发现使用DAA治疗HCV感染与VZV再激活风险增加之间存在关联的证据。
原文出处
Rohde MD, Tracy L, Komatsu TE, El-Kamary SS, Carter W,No Association Between DAA Treatment for HCV Infection and Herpes Zoster Infection in Analysis of Data From 37 Clinical Trials.Clin Gastroenterol Hepatol 2021 Aug;19(8)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CGH#
28
#VZV#
25
#再激活#
31
#HCV#
46
#DAA#
47
#HCV感染#
30