Blood:影响B-ALL患者博纳吐单抗治疗效果的肿瘤内外标志物
2020-09-15 QQY MedSci原创
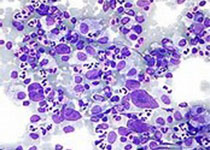
Blinatumomab(博纳吐单抗),是一种靶向CD3+T细胞和CD19+肿瘤细胞的双特异性抗体,在B祖细胞急性淋巴细胞白血病(B-ALL)中显示出不同的疗效。
为了明确决定反应性的肿瘤内外源因子,Zhao等人采用单细胞测序研究了44位采用博纳吐单抗治疗的复发性/难治性B-ALL成人患者(包括2例MRD阳性的患者)。
血液病患者的总有效率为55%,携带CRLF2重排的费城染色体(Ph)样ALL患者的有效率较高(12/16, 75%)。应答者的预处理样本表现出了免疫反应增强的肿瘤内转录特征。
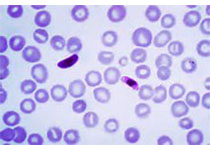
多重机制导致CD19表达缺失,包括CD19基因突变、CD19突变性等位基因特异性表达、低CD19 RNA表达和CD19信号复合体伙伴CD81突变。低二倍体患者由于非整倍体介导的非突变性CD19等位基因丢失,容易出现CD19阴性型复发。
在基线或治疗期间,2号外显子剪切变异的CD19亚型(CD19 ex2part)表达增加与治疗失败有关。
本研究表明,肿瘤内在和外在的因素均可影响患者对博纳吐单抗治疗的反应性。CD19突变常见于博纳吐单抗治疗期间CD19阴性型复发的患者。检测CD19 ex2part剪切变异代表了一种预测博纳吐单抗治疗失败的新型生物标志物。
原始出处:
Yaqi Zhao, et al. Tumor intrinsic and extrinsic determinants of response to blinatumomab in adults with B-ALL. Blood. September 3, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#标志物#
22
#治疗效果#
27
#ALL#
22
#博纳吐单抗#
38
#B-ALL#
41
学习了
81
学习
87
谢谢梅斯提供这么好的信息,学到很多
35
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
42
棒棒哒
89