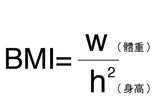
ASCO 2016:转移性结直肠癌患者BMI越高,生存越好?
2016-06-05 Seven L 译 MedSci原创
ASCO年会上的一项荟萃分析结果显示,与正常体重患者相比,超重和肥胖的转移性结直肠癌患者有更长的OS。此外BMI<18.5的患者经历了显着恶化的OS和PFS。来自法国Avicenne医院的Thomas Aparicio博士说:“我们的分析结果证实了先前的研究结果,肥胖提高转移性结直肠癌患者的生存。值得注意的是,贝伐单抗对肥胖和非肥胖患者的有效性是一致的,但改善肥胖患者预后的原因仍然是未知的;有人认
ASCO年会上的一项荟萃分析结果显示,与正常体重患者相比,超重和肥胖的转移性结直肠癌患者有更长的OS。此外BMI<18.5的患者经历了显着恶化的OS和PFS。
来自法国Avicenne医院的Thomas Aparicio博士说:“我们的分析结果证实了先前的研究结果,肥胖提高转移性结直肠癌患者的生存。值得注意的是,贝伐单抗对肥胖和非肥胖患者的有效性是一致的,但改善肥胖患者预后的原因仍然是未知的;有人认为免疫调节或化疗耐受性可能是一个因素。”
以前的研究显示,早期结直肠癌癌患者中,有高或低的BMI与预后不良相关,低BMI与转移性结直肠癌预后不良相关。
Aparicio和他的同事评估了不同时间点BMI对转移性结直肠癌患者预后的影响,同事评估BMI与治疗剂量间的联系。研究分析了1991-2013年间的2085例转移性结直肠癌患者。数据显示,20%的患者肥胖(BMI > 30),其中1991-1999占7.7%,2000-2006占14.5%,2007-2013占13.6%。
研究者根据BMI将患者分为肥胖(BMI 30)以及正常或超重,此外还分为极瘦(BMI < 18.5)或非极瘦(BMI > 18.5)。
分析结果显示,与正常和超重患者(BMI, 18.5 -29)相比,肥胖患者经历了较长时间的中位OS(19.5 个月 vs. 16.6 个月; HR = 1.15; 95% CI, 1-1.33),但是中位数PFS在两组没有差异(7.9 个月 vs. 7.3 个月; HR = 1.06; 95% CI, 0.93-1.22),客观缓解率(ORR)也没有差异(42% vs. 38.5%; OR = 1.02; 95% CI, 0.77-1.37)。
当研究人员以BMI 25为界时评估患者,他们发现更高BMI的患者的OS显著延长(18.5个月 vs. 16.3个月;HR = 1.13;95% CI,1.02-1.25),ORR也更高 (42% vs. 36%; OR = 1.23; 95% CI, 1.01-1.5)。
亚组分析结果显示,“肥胖”可以改善男性患者的OS(P = .03)和PFS(P = .05)。而BMI小于18.5的患者有较低的OS(HR,0.75;95% CI,0.6-0.94)和PFS(HR,0.75;95% CI,0.6-0.93)。与正常或超重患者相比,肥胖患者在第一周期经历药物剂量减少的比例更大(34% vs. 17%; P < .001)。
作者说:“研究的一个局限在于缺乏详细的肥胖和生物学数据,在以后还需要对BMI与转移性结直肠癌患者的联系进行进一步详细的研究。”
原始出处:
Aparicio T, et al. Abstract 3532. Presented at: ASCO Annual Meeting; June 3-7, 2016; Chicago.
Higher BMI linked to improved survival for patients with metastatic colorectal cancer.Healio.June 4, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASC#
36
不错哦,会学到很多
74
#转移性#
34
#结直肠#
43
这样也行
116
很不错啊
126
不错的文章,多学习
125