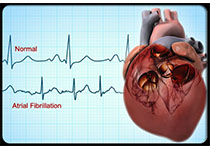
Circulation:植入ICD的患者房性心律失常时,应用外部还是内部心脏复律来转复窦性心律?
2019-09-26 MedSci MedSci原创
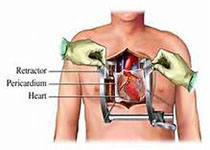
房性心律失常在植入式心律转复除颤器(ICD)患者中很常见。体外冲击和通过指令ICD冲击的内部电复律被用于心律控制。但关于外部心脏复律和内部心脏复律的效果,以及导线或设备故障的风险,目前缺乏确切的数据。研究人员推测外部心脏复律的安全性不次于内部心脏复律,而成功恢复窦性心律的概率优于内部心脏复律。并开展试验对此进行验证。研究人员从13个医疗中心招募接受选择性心脏复律治疗房性心律失常的患者,将其按1:1
研究人员从13个医疗中心招募接受选择性心脏复律治疗房性心律失常的患者,将其按1:1随机分至内部或外部心脏复律。主要安全指标是导线或设备故障的综合。主要疗效指标是房性心律失常转复窦性心律。
共招募了230位患者,随机分至两组。外部和内部心脏复律组的电击有效率分别为93%和65%(p<0.001)。两组均未观察的临床相关的不良事件。3例预先存在的导线故障导致导线复律失败。两组间的肌钙蛋白释放无差别。
本研究是第一个在ICDs患者中对比外部心脏复律和内部心脏复律的随机对照试验。外部心脏复律转复窦性心律的效果更好。
原始出处:
Jakob Lüker, et al.Internal Versus External Electrical Cardioversion of Atrial Arrhythmia in Patients With Implantable Cardioverter-Defibrillator.Circulation. 2019;140:1061–1069
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心脏复律#
35
#房性心律失常#
39
#转复窦性心律#
18
#ICD#
0
#窦性心律#
37
#植入#
35