J Urol:膀胱切除术前新辅助化疗对肌肉浸润性膀胱癌的病理分期和生存预后的益处
2021-05-28 Nebula MedSci原创
新辅助化疗与所有组织学变异类型的肌肉浸润性膀胱癌的病理分期下调相关,还多种组织亚型的患者的OS改善相关
膀胱癌是男性第4常见的癌症,在所有人群中的发病率排名第6,占全部癌症病例的4.4%。组织学变异的肌肉浸润性膀胱癌 (MIBC) 患者的预后较差。目前尚不清楚根治性膀胱切除术前新辅助化疗是否与组织学变异患者的病理分期下降或总生存期 (OS) 改善有关。
本研究旨在评估组织学变异MIBC患者接受新辅助化疗与病理分期下降和OS之间的关联。
研究人员从国家癌症数据库中筛查了2004年-2017年接受根治性膀胱切除术的无转移的MIBC患者。按组织学亚组、有无接受新辅助化疗进行分层。病理分期下降定义为pT0N0或pT≤1N0,OS位从确诊到死亡或最后随访的时间。采用多变量逻辑回归分析新辅助化疗与病理分期下降之间的关联。采用多变量Cox回归分析确定新辅助化疗与OS之间的关联。
最终研究人群 纳入了31218例患者:尿路上皮癌(UC): 27779例; 肉瘤样UC: 501例; 微乳头状UC: 418例; 鳞状细胞癌(SCC): 1141例; 神经内分泌癌: 629例; 腺癌: 750例。
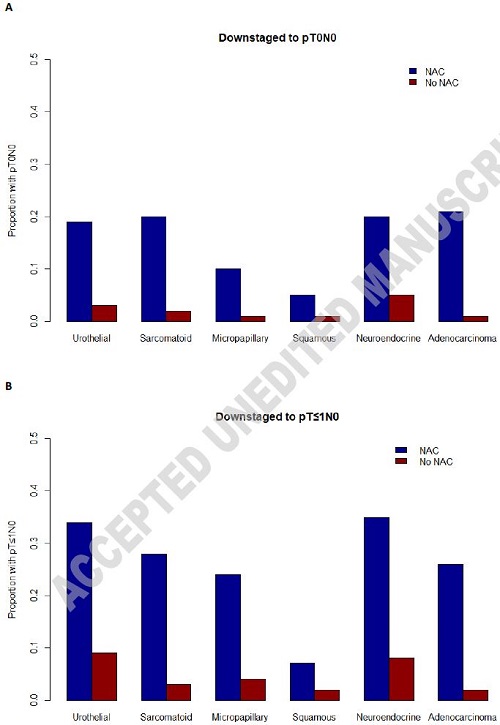
有无新辅助化疗的患者的病理分期下调情况
在所有组织学亚组中,新辅助化疗与病理分期下调至pT0N0相关(UC的优势比[OR]:5.1[95%CI 4.6-5.6]; 肉瘤样UC:13.8 [5.5-39.0]; 微乳头状UC:9.7 [2.8-46.8]; SCC:7.4 [2.1-24.5]; 神经内分泌:4.7 [2.6-9.2]; 腺癌:23.3 [8.0-74.2])。
新辅助化疗与UC (HR 0.8 [0.77-0.84])、肉瘤样UC (HR 0.64 [0.44-0.91]) 和神经内分泌癌 (HR 0.55 [0.43-0.70]) 患者的OS改善相关。
总之,新辅助化疗与所有组织学变异类型的MIBC的病理分期下调相关,还与UC、肉瘤样UC和神经内分泌癌患者的OS改善相关。
原始出处:
Chakiryan Nicholas H,Jiang Da David,Gillis Kyle A et al. Pathologic Downstaging and Survival Outcomes Associated with Neoadjuvant Chemotherapy for Variant Histology Muscle Invasive Bladder Cancer. J Urol, 2021, undefined: 101097JU0000000000001855.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#切除术#
37
#新辅助#
42
#生存预后#
35
#病理分期#
36
#膀胱切除术#
45
积极评论
56
膀胱癌真怪,明明是免疫敏感性肿瘤,为什么PD-1治疗效果不好呢?难道靶点不对?将来CD47会不会有效
55