Eur Urol:将勃起功能恢复的年龄差异考虑入根治性前列腺切除术的利弊。
2017-08-31 fengxiangxin MedSci原创
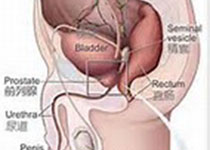
尽管主动监测越来越多地应用于低危前列腺癌患者的管理中,但许多符合条件的患者仍然接受了手术治疗。患者考虑手术而不是主动监视的一个原因是存在这样一个论点:术后勃起功能的恢复可能性是年龄依赖性的,也就是说,延迟手术的患者可能失去手术后恢复勃起功能的机会。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#切除术#
25
#利弊#
30
#前列腺切除#
29
#勃起#
27
#勃起功能#
23
#根治#
29
#功能恢复#
40