J Clin Oncol:Eprenetapopt联合阿扎胞苷治疗TP53突变型MDS和AML
2021-02-19 MedSci原创 MedSci原创
Eprenetapopt(APR-246)是一种新型的一类药物,可使p53蛋白重构,并重新激活其促凋亡和细胞周期阻滞的功能
无论采取怎样的治疗,TP53突变(TP53m)的骨髓增生异常综合症(MDS)和急性髓系白血病(AML)的预后均非常差,阿扎胞苷(AZA)单药治疗的缓解率仅40%(完全缓解率[CR] 20%),且缓解持续时间短,中位总生存期(OS)大约只有6个月。Eprenetapopt(APR-246)是一种新型的一类药物,可使p53蛋白重构,并重新激活其促凋亡和细胞周期阻滞的功能。
本研究是一项II的临床试验,旨在评估Eprenetapopt联合AZA用于未治疗过的高或非常高的国际预后评分系统R的TP53m MDS和AML患者的安全性和有效性。
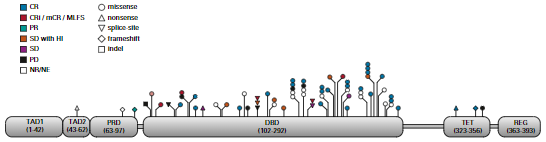
所有患者基线时的TP53突变情况
共招募了52位TP53m 患者(34位 MDS、18位AML)。在MDS患者中,总缓解率(ORR)达到62%,包括47%的CR,中位缓解持续时间达到10.4个月。在AML患者中,ORR为33%,包括17%的CR。
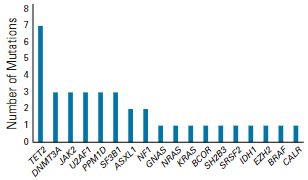
伴发体细胞突变
73%的缓解患者获得TP53二代测序阴性(如变异等位基因频率<5%)。主要的治疗相关不良反应有发热性中性粒细胞减少(36%)和神经系统不良事件(40%),后者与治疗开始时肾小球滤过率较低(P <0.01)和年龄较大(P =0.05)相关;适当降低Eprenetapopt剂量后,暂时性停药得以解决且未见复发。
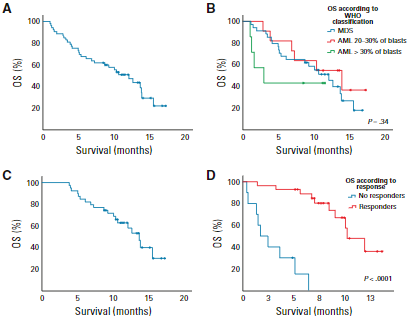
患者预后
中位随访9.7个月时,MDS患者的中位OS达到12.1个月,AML患者的OS达到3.0个月。
总而言之,在非常高风险的TP53m MDS和AML患者中,Eprenetapopt与AZA的联合方案安全性好,展现出了比单用AZA更高的ORR和CR率以及更长的OS。
原始出处:
Thomas Cluzeau, et al. Eprenetapopt Plus Azacitidine in TP53-Mutated Myelodysplastic Syndromes and Acute Myeloid Leukemia: A Phase II Study by the Groupe Francophone des Myélodysplasies (GFM). Journal of Clinical Oncology. February 18, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#突变型#
55
#Oncol#
58
#NET#
46
#MDS#
42
#J Clin Oncol#点击查看更多该期刊内容
82
#p53#
44
#TP53#
50
学习了,涨知识了!
85
谢谢梅斯分享这么多精彩信息
62
学习了
88