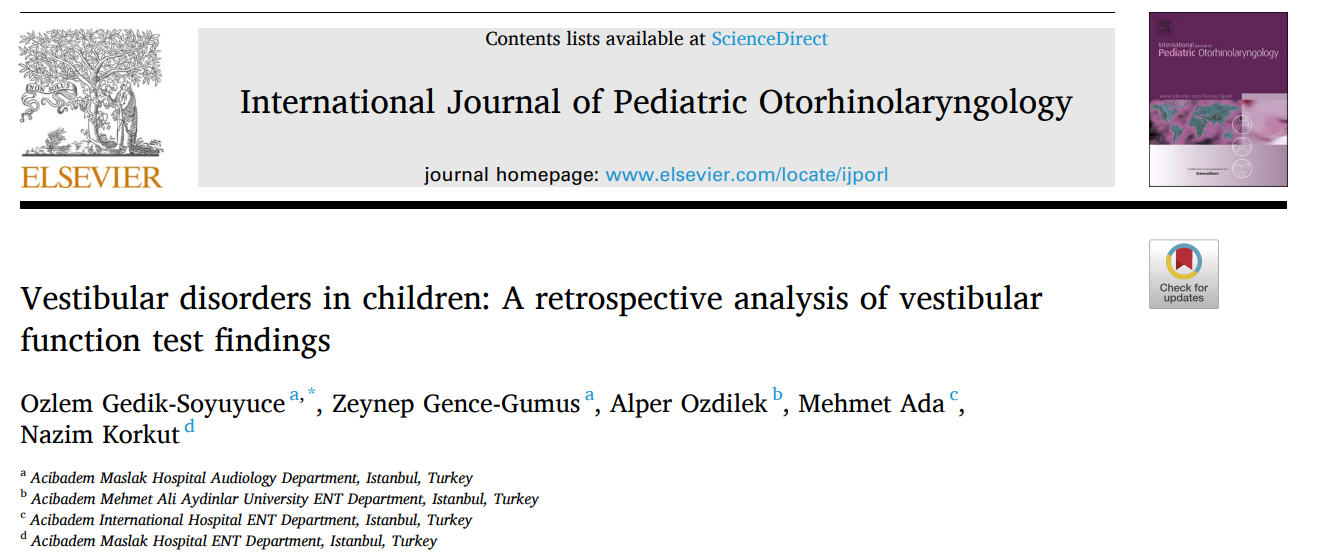
Int J Pediatr Otorhinolaryngol:儿童前庭功能障碍的回顾性分析
2021-05-24 AlexYang MedSci原创
儿童眩晕使小儿前庭疾病的诊断复杂化,其表现形式也不清楚。眩晕和头晕在儿童中可表现为偏头痛、神经系统疾病、肠道疾病、眼科疾病或前庭病变。小儿眩晕在现代科学文献中首次由哈里森于1962年提及。由于听觉和前
儿童眩晕使小儿前庭疾病的诊断复杂化,其表现形式也不清楚。眩晕和头晕在儿童中可表现为偏头痛、神经系统疾病、肠道疾病、眼科疾病或前庭病变。小儿眩晕在现代科学文献中首次由哈里森于1962年提及。由于听觉和前庭病变的同时存在,新生儿听力筛查项目广泛的普及提高了人们对小儿前庭病变的认识。在美国,每年每1000个出生的婴儿中,有2到3个有听力障碍,其中20%-70%有前庭障碍。
近期,有研究人员阐述了儿童中最常见的前庭障碍及其在前庭功能测试中的相关结果。
研究人员在3400名进行前庭评估的患者中收集了203名儿童的数据,这些患者在一家三级医院的眩晕中心接受了3年的前庭评估。儿童的平均年龄为11.16±3.87(范围,1-17)岁,并对进行了回顾性的数据分析。
结果发现,在3400名患者的203名儿童中,有78.3%(n=159)诊断为前庭障碍,表明他们研究队列的3年的发病率为4.67%。良性阵发性位置性眩晕(BPPV)是他们研究中儿童队列最常见的诊断(49%;n=100),其中包括原发性BPPV和与其他前庭病症相关的继发性BPPV。前庭偏头痛(VM)是第二大常见的诊断(41%;n=83),其次是儿童良性阵发性眩晕(BPVC;4.5%,n=9),前庭神经炎(VN;4.5%,n=9),和精神性眩晕(4.5%,n=9)。研究结果还显示,美尼尔病(MD;1.5%,n=3)和中枢性眩晕(1.5%,n=3)在儿童中较少诊断。只有1名儿童诊断为外淋巴瘘(PLF),并经手术证实。
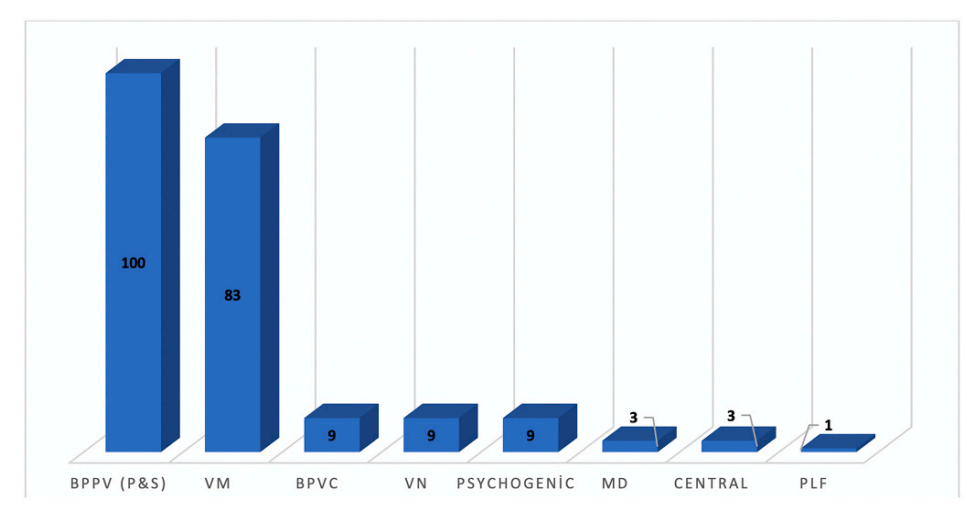
159名前庭障碍儿童的诊断分布
综上所述,BPPV和VM是他们研究中最常见的小儿前庭疾病。临床医生应该了解最常见的儿童前庭疾病的发病率、体征和症状,以便于诊断、治疗和康复。另外,通过进行与年龄相适应的前庭功能测试,能够改善鉴别诊断,从而指导医学治疗和康复。
原始出处:
Ozlem Gedik-Soyuyuce, Zeynep Gence-Gumus , Alper Ozdilek et al. Vestibular disorders in children: A retrospective analysis of vestibular function test findings. Int J Pediatr Otorhinolaryngol. 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
42
#前庭功能障碍#
46
#DIA#
41
#功能障碍#
40
#回顾性分析#
42
#前庭功能#
32