Rheumatology:系统性硬化相关性肺动脉高压患者重复入院的相关风险因素
2021-07-20 MedSci原创 MedSci原创
与SSc-PH患者12个月内再入院相关的最强预测因素是与PH相关的住院指标
系统性硬化(SSc)是一种以炎症、纤维化和血管病变为特征的自身免疫性疾病,肺动脉高压(PH)是SSc患者死亡的主要原因之一。WHO根据肺压力和病因将PH分成⑤组:
第1组:肺动脉高压(PAH);第2组:肺静脉高压;第3组:伴有呼吸系统疾病或低氧血症的肺动脉高压;第4组:慢性血栓性或栓塞性疾病引起的肺动脉高压;第5组:其他原因(如硬化症)引起的肺动脉高压。
本研究旨在确定与系统性硬化症相关的肺动脉高压 (SSc-PH) 患者再入院相关的个体水平因素。
招募了参加肺动脉高压评估和硬化症预后评估(PHAROS)注册的患者,采集了与SSc-PH疾病严重程度和住院率相关的临床数据。再入院定义为出院后12个月内再次住院。使用Fisher精确检验、Wilcoxon秩和检验或Kruskal Wallis 检验比较有无再入院个体的特征。
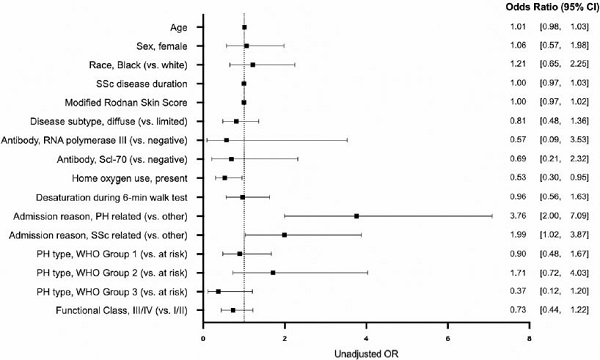
12个月内再入院的风险因素的优势比
在PHAROS登记的572位SSc-PH患者中,54%的患者于2015年至2016年期间住院1次或以上。在曾经住院过的个体中,34%的个体再入院≥1次。与无再入院的个体相比,有再入院经历的个体首次住院和下次PHAROS就诊之间的间隔中位时间较短(37 vs 81天;p<0.001)。与PH或SSc相关的指数入院与12个月内再入院的几率增加有关(aOR分别是6.6和2.2)。与非家庭氧气用户相比,家庭氧气用户再入院的可能性较小(aOR 0.44)。最后,种族、年龄、相比、病程长短和疾病亚型均与再入院风险无关。
综上所述,与SSc-PH患者12个月内再入院相关的最强预测因素是与PH相关的住院指标。家庭氧气的使用可降低再入院的几率。未来研究应明确是否需要通过家庭氧气来降低SSc-PH患者的再入院风险。
原始出处:
Showalter Kimberly,Pinheiro Laura C,Jannat-Khah Deanna et al. Hospital readmission in systemic sclerosis associated pulmonary hypertension: Results from the PHAROS registry.[J] .Rheumatology (Oxford), 2021, https://doi.org/10.1093/rheumatology/keab569
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肺动脉高压患者#
0
#相关性#
36
#动脉高压#
28
#系统性#
46
#Rheumatology#
35
#系统性硬化#
27
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
44