Ann Oncol: 纳武利尤单抗(Nivolumab)二线治疗并不能改善小细胞肺癌的预后:来自CheckMate 331临床研究
2021-06-01 yd2015 MedSci原创
纳武利尤单抗(Nivolumab)对比化疗二线治疗并不能改善复发小细胞肺癌的预后。没有发现新的不良事件发生。亚组分析发现,某些选择性的患者可能可以从纳武利尤单抗取得OS的获益。
小细胞肺癌(SCLC)对放化疗较敏感,一线治疗时缓解率较高,但是几乎都要经历复发。而复发的小细胞肺癌选择的药物比较有限。I/II期临床研究发现纳武利尤单抗(nivolumab)对既往治疗进展的SCLC有效。因此,研究者开展了III期临床研究CheckMate 331,评估纳武利尤单抗(nivolumab)对比化疗二线治疗SCLC的疗效和安全性,近期,研究成果发表在了Annals of Oncology杂志上。

该研究是全球的开放标签、随机对照III期临床研究(ClinicalTrials.gov number,NCT02481830)。纳入一线治疗后复发的SCLC患者。主要研究终点为总生存期(OS),次要终点为研究者评估的无进展生存(PFS),客观缓解率(ORR)和持续缓解时间(DOR)。
研究共纳入了569例患者,其中284例患者随机分配到纳武利尤单抗(nivolumab)组治疗,285例患者随机分配到化疗组治疗。两组的中位随访时间分别为7.0和7.6个月。对于OS分析,最短随访时间为15.8个月。两组的中位OS并没有明显差异,为7.5个月vs8.4个月(HR=0.86,95%CI 0.72-1.04,P=0.11)。亚组分析发现,只有基线时乳酸脱氢酶(LDH)小于等于正常上限值(ULN)(HR, 0.70; 95% CI, 0.53-0.90)和没有肝转移(HR, 0.77; 95% CI, 0.61-0.97)患者能够从纳武利尤单抗治疗取得OS获益。中位PFS分别为1.4个月(95% CI, 1.4-1.5)和3.8个月(95% CI, 3.0-4.2)(HR, 1.41; 95% CI, 1.18-1.69)。两组6个月和12个月PFS率分别为19.7%和26.5%,以及10.9%和10.0%。
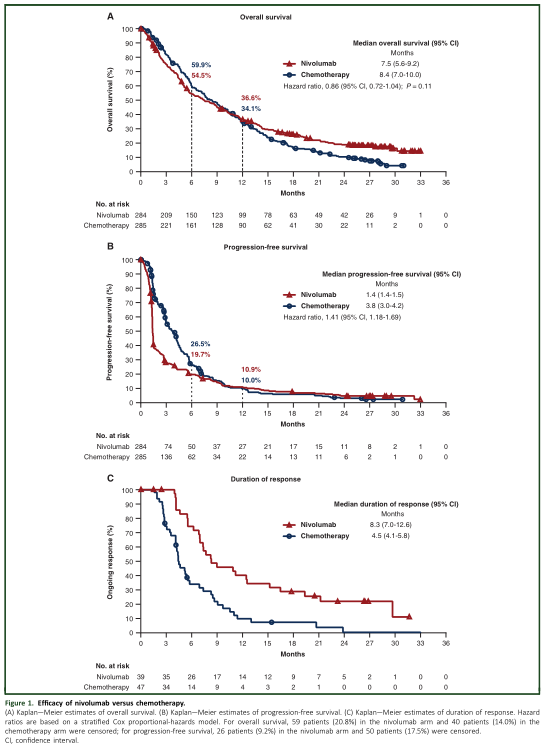
两组的OS、PFS和DOR分析
两组的ORR分别为13.7%和16.5%(odds ratio, 0.80; 95% CI, 0.50-1.27)。中位缓解持续时间分别为8.3个月(95% CI,7.0-12.6)和4.5个月(95% CI,4.1-5.8)。
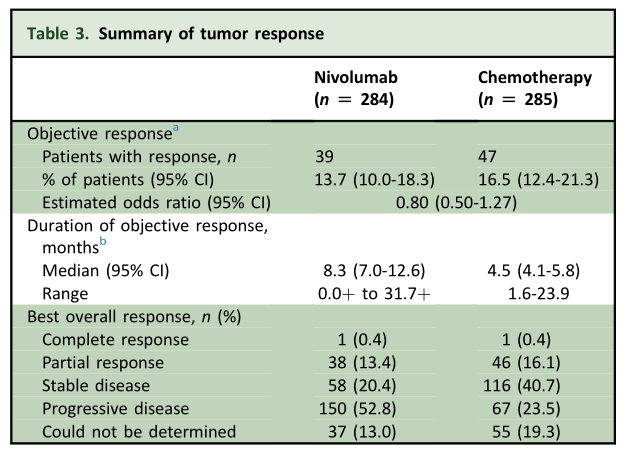
两组治疗ORR和DOR
根据PDL1表达水平分组分析时,PDL1 CPS ≥ 1% 时,纳武利尤单抗和化疗组的中位OS分别为7.0和8.6个月(HR= 0.96,95% CI, 0.67-1.38);中位PFS分别为1.5和4.3个月(HR=1.52, 95% CI, 1.06-2.19)。PDL1 CPS < 1% 时,纳武利尤单抗和化疗组的中位OS分别为7.3和8.1个月(HR= 0.91,95% CI, 0.66-1.25);中位PFS分别为1.4和4.1个月(HR=1.68, 95% CI, 1.23-2.31)。

根据PDL1分层分析两组OS和PFS
两组任何级别治疗相关不良事件(TRAEs)发生率分别55.3%和90.2%,包括3级或4级事件分别为13.8%和73.2%。与化疗相比纳武利尤单抗组发生严重TRAEs的比例也较低(13.1% vs 32.8%)。两组TRAEs导致治疗中断的比例分别为6.0% 和 14.3%。纳武利尤单抗治疗最常见的TRAEs是内分泌(11.7%)、皮肤(11.3%)和胃肠道(7.1%)相关事件。
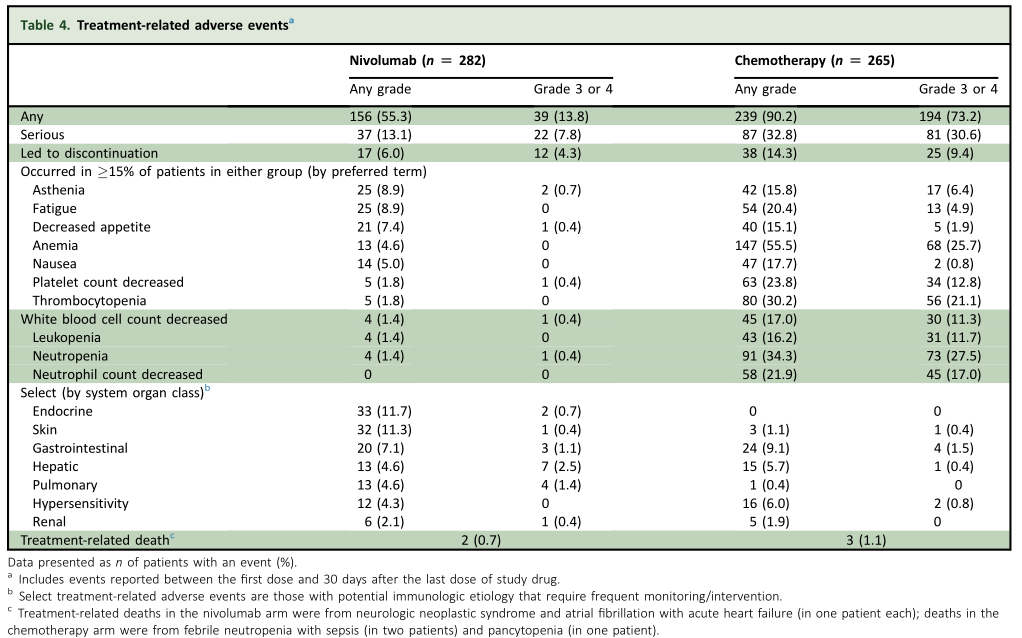
治疗相关不良事件
综上: 纳武利尤单抗(Nivolumab)对比化疗二线治疗并不能改善复发小细胞肺癌的预后。没有发现新的不良事件发生。亚组分析发现,某些选择性的患者可能可以从纳武利尤单抗取得OS的获益,比如基线时乳酸脱氢酶(LDH)小于等于正常上限值(ULN)和没有肝转移患者。
原始出处:
D R Spigel, D Vicente, T E Ciuleanu, et al. Second-line nivolumab in relapsed small-cell lung cancer: CheckMate 331. Ann Oncol. 2021 May;32(5):631-641. doi: 10.1016/j.annonc.2021.01.071. Epub 2021 Feb 1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












值得学习
33
#NIV#
47
#Checkmate#
46
#mAb#
42
#Oncol#
37
#二线治疗#
35
厉害👍🏻
67
谢谢梅斯分享这么多精彩信息
52