胰腺癌新突破:G-CSF抑制剂有望逆转胰腺癌!
2017-09-04 佚名 medicalxpress
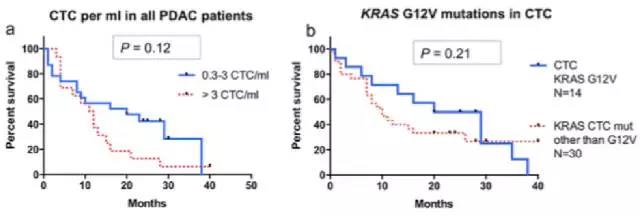
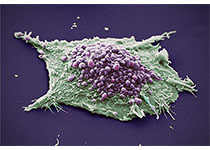
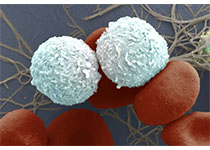
胰腺导管癌指的是始于胰腺导管上皮或腺泡细胞的实质性癌,也是胰腺肿瘤中最多见者。胰腺导管癌(PDAC)是最致命的癌症之一,有些研究表示,慢性胰腺炎和糖尿病是胰腺癌的病因所在,也有些研究并不支持这一观点。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#抑制剂#
39
#新突破#
41
#G-CSF#
57
#CSF#
38
学习了.谢谢分享
78