Chest:降低COPD恶化风险与FEV1的改善相关!
2017-05-11 xing.T MedSci原创
该研究的结果表明,FEV1增加与较低COPD恶化风险显著相关,提示气道通畅是这一效应的一个重要机制。
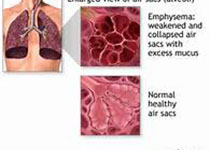
不同种类的药物降低COPD加重风险的机制尚不清楚。近日,胸部疾病领域权威杂志Chest杂志上发表了一篇荟萃分析文章。研究人员假设1秒用力呼气量(FEV1)可以用来衡量降低的COPD恶化风险和改善气道通畅之间的相关性。
研究人员通过对多个数据库进行检索以及系统的文献评价,确定了在文献中报道了剂量前FEV1(dFEV1)治疗变化和发生中度至重度急性加重的COPD临床试验。利用Meta回归分析,构建了一个以dFEV1作为调节变量的模型,并以恶化率(RD)的绝对差异、发作率比(RR)或风险比(HR)作为因变量。
研究人员分析了119227例受试者的RD和RR,以及73475例患者的HR。dFEV1每变化100毫升,HR下降了21%(95%可信区间为17-26 %,P<0.001,R2=0.85),以及绝对的恶化率下降了0.06次每名患者每年(95%可信区间为0.02-0.11,P=0.009,R2=0.05),这对应的RR为0.86(95%可信区间为0.81-0.91,P<0.001,R2=0.20)。在多个亚组分析中,与恶化风险的相关性仍具有统计学意义。
该研究的结果表明,FEV1增加与较低COPD恶化风险显著相关,提示气道通畅是这一效应的一个重要机制。
原始出处:
Alexander D. Zider,et al. Reduced COPD exacerbation risk correlates with improved FEV1: A meta-regression analysis.Chest. 2017. http://journal.publications.chestnet.org/article.aspx?articleid=2627080
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#FEV1#
42
#Chest#
40
#FEV#
28
#EST#
41
谢谢分享,学习了
62
谢谢分享,学习了!
63
学习了感谢分享
66
非常好的文章,学习了,很受益
55
改善copd患者fev1,可改善患者病情恶化风险
65
谢谢分享,学习了
36