Chest:COPD-OSA重叠综合征
2017-04-28 MedSci MedSci原创
慢性阻塞性肺疾病(COPD)和阻塞性睡眠呼吸暂停综合征(OSA)是常见的两种疾病,这也意味着,基于机会联合,这两种疾病合并发生(重叠综合征)可能也是常见的。然而,COPD不同的临床表型影响着共存的OSA的可能性,因为与肺气肿表型相关一些因素,如增加的肺容积和低体重指数(BMI)对OSA的发生具有一定的预防作用,而与慢性支气管炎表型相关的外周水肿和BMI的增加又可以促进OSA的发生。COPD和OSA
慢性阻塞性肺疾病(COPD)和阻塞性睡眠呼吸暂停综合征(OSA)是常见的两种疾病,这也意味着,基于机会联合,这两种疾病合并发生(重叠综合征)可能也是常见的。
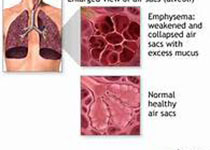
然而,COPD不同的临床表型影响着共存的OSA的可能性,因为与肺气肿表型相关一些因素,如增加的肺容积和低体重指数(BMI)对OSA的发生具有一定的预防作用,而与慢性支气管炎表型相关的外周水肿和BMI的增加又可以促进OSA的发生。
COPD和OSA的发生都与类似的生理和分子结果相关,如缺氧和全身炎症,这些有助于心血管和其他并发症的发生,同时,肺动脉高压在重叠综合征患者中也是高度普遍的。
然而,目前为止,仅有很少报告研究评估了重叠征患者的全身炎症和其他心血管并发症。 OSA在COPD患者中的诊断需要对相关临床特征的认识,筛查调查表可能有助于确定合适的患者进行进一步的夜间睡眠监测。
在COPD患者中共同存在的OSA的认识具有重要的临床意义,因为重叠综合征患者的治疗与单独的COPD不同,并且没有用夜间气道正压通气治疗的重叠患者的生存率显着低于适当治疗的重叠患者。
原始出处:
McNicholas WT. COPD-OSA Overlap Syndrome: evolving evidence regarding epidemiology, clinical consequences, and management. Chest. 2017 Apr 22. pii: S0012-3692(17)30742-0. doi: 10.1016/j.chest.2017.04.160.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#EST#
0
#Chest#
0
学习了,谢谢作者分享!
0
#OSA#
34
#综合征#
28