Annals Neurology:复旦大学俞金泰-淀粉样蛋白-Tau-神经退行性框架在认知健全的成年人中的应用
2022-07-17 Freeman MedSci原创
该研究揭示了中国北方认知完整的汉族人群中A,D连续体的分布和潜在的风险因素
作为痴呆症最常见的原因,阿尔茨海默氏病(AD)已成为国际上的一个优先事项。然而,尽管经过几十年的研究,仍然没有药物能够有效地治愈AD或减缓AD的进展。这种严峻的形势加强了对AD二级预防的重要性。
 图1: 论文封面图
图1: 论文封面图
AD的核心病理特征是细胞外淀粉样斑块的堆积、tau细胞内神经纤维缠结、神经变性和突触丧失。目前的共识是,AD的发展是缓慢和渐进的,在几年到几十年的无症状过程中,上述病症已经发生。因此,将临床前的AD患者与认知完整的人群区分开来并探索他们的风险因素成为二级预防策略的两个关键问题。
令人鼓舞的是,随着生物标志物的发展,AD的核心病理变化可以在体内检测到,甚至在临床前阶段。因此,AD诊断的重点已经从临床症状转移到生物标志物框架。2018年,美国国家老龄化研究所和阿尔茨海默氏症协会进一步提出了AT(N)框架,将AD相关的生物标志物分为三个二元类:大脑淀粉样蛋白沉积(A),tauopathy(T),以及神经变性或神经元损伤(N)。这个拟议的研究框架已经发展到将AD的概念化,认为它是一个疾病的连续体,有独立于临床表现的淀粉样蛋白相关病理的证据。基于这一框架,有必要揭示AD连续体在不同群组和种族中的认知完整人群中的分布。值得注意的是,尽管已经发表了一些基于美国或欧洲为中心的队列的研究,但对这个框架在亚洲人群中的表现知之甚少。由于不同人群在遗传因素、生活习惯和社会背景方面存在巨大差异,本研究在亚洲人群中可能提供新的见解。
此外,根据世界卫生组织关于降低认知能力下降和痴呆风险的指南,以前已经确定了一些AD痴呆阶段的风险因素。然而,以前的研究大多是基于临床诊断,缺乏基于生物标志物诊断的大型研究。在认知完整阶段,哪些因素仍被赋予类似的优先权,仍有待于在AT(N)框架下确定。
藉此,复旦大学的俞金泰团队:
(1)评估AT(N)分类方案在中国北方汉族人群大型认知完整队列--中国阿尔茨海默病生物标志物与生活方式(CABLE)队列中的理论分布和认知表现;
(2)探索基于AT(N)框架的AD连续性的早期不可改变和可改变的风险因素,这可能为帮助临床前诊断和定向招募AD干预提供一个重要机会。
该研究通过AT(N)方案对认知完整的中国阿尔茨海默病生物标志物和生活方式(CABLE)参与者进行分类。使用高斯混合模型确定脑脊液生物标志物的临界值,该临界值区分了1,005名参与者(平均年龄61岁;40%为女性)的AD连续性(A+T-N-、A+T+N-、A+T-N+和A+T+N+)。多变量逻辑回归和Cochran-Armitage趋势测试被用来测试神经心理学表现和AD连续性的风险因素。
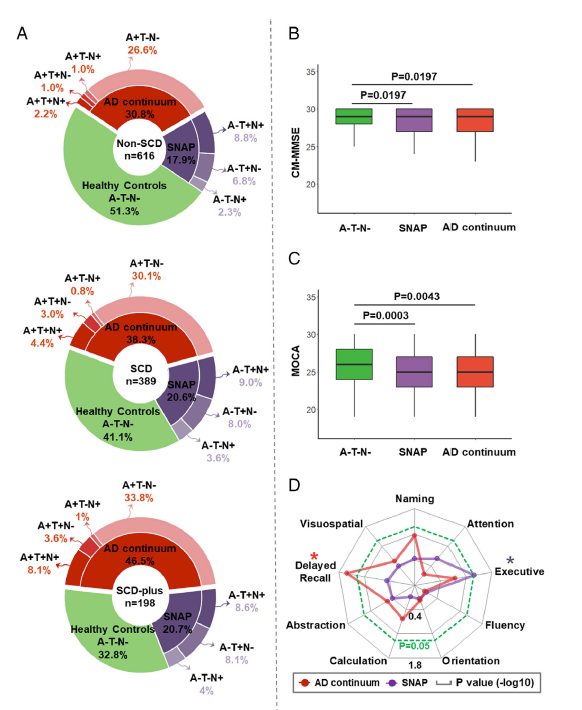 图2:论文结果图
图2:论文结果图
他们发现:约有三分之一的人(33.7%)属于AD连续体。四个潜在的可改变的风险因素,包括高血压、甲状腺疾病、社会隔离和最小的抑郁症状,被确定为AD连续体(OR范围为1.68-6.90)。
AD连续体的流行趋势与更多的风险因素有关(趋势的P<0.0001)。每增加一个可改变的危险因素,AD连续体的风险就增加约2倍(OR 1.9,95% CI 1.65-2.24,P <0.0001)。
该研究揭示了中国北方认知完整的汉族人群中AD连续体的分布和潜在的风险因素,填补了该地区关于AT(N)框架在亚洲人群中表现的空白。
原文出处:
Hu H, Bi Y, Shen X, et al. Application of the Amyloid/Tau/Neurodegeneration Framework in Cognitively Intact Adults: The CABLE Study. _Annals of Neurology_. Published online July 4, 2022:ana.26439. doi:[10.1002/ana.26439](https://doi.org/10.1002/ana.26439)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#Neurol#
32
#神经退行#
41
#淀粉样蛋白#
53
#Tau#
51
#复旦#
36