IBD:肛周克罗恩病患者抗TNF治疗之前并不需要麻醉下的瘘管探查
2022-07-17 xuyihan MedSci原创
肛瘘是临床上难以自愈的一种肛周感染性疾病,是由内口、外口以及连接两者的瘘管相组成。一般来说,这些瘘管是由于长期炎症刺激,将肛内的分泌物,通过瘘管排泄到肛门外,在排泄过程中又形成了局部脓肿。
肛周瘘管病是克罗恩病最常见和最难治疗的表型之一。国际指南建议采用多学科治疗方法,主要是通过麻醉检查 (EUA) 进行瘘管引流,然后使用肿瘤坏死因子 (TNF) 抑制剂进行药物治疗。EUA允许引流存在脓肿的瘘管,同时建议插入宽松的挂线以防止脓肿复发。这种策略不仅被认为是肛周克罗恩病初始治疗的重要组成部分,而且还可以提高抗 TNF 治疗的有效性。因此,本项研究的主要目标是比较EUA-抗TNF联合治疗方法与单独抗TNF治疗对肛周克罗恩病的有效性。

研究人员在2009年至2019年之间进行了一项比较队列研究。将在抗TNF治疗(联合模式治疗)之前接受 EUA 治疗的肛周克罗恩病患者与单独的抗TNF进行了比较。主要观察结果是临床评估的瘘管闭合情况。次要观察结局包括随后的局部手术和粪便转移。最后研究人员进行了针对脓肿、伴随免疫调节剂和抗 TNF 起始时间调整的多变量分析。
在155名患者中总共有188次抗TNF治疗,其中66 名(35%)在 EUA 之后。脓肿(50% VS 15%;P < .001)和伴随的免疫调节剂治疗(64% VS 50%;P= .07)在联合治疗组中更为常见,而年龄、吸烟状况、病程和肠道疾病位置无显着差异。在 3个月和12个月的随访时间中联合治疗与较高的瘘管闭合率无关(调整优势比 [aOR],0.7;95% 置信区间 [CI],0.3-1.8)。在随访4.6年后,联合治疗与随后的局部手术干预相关(调整后的风险比,2.2;95% CI,1.3-3.6),但与粪便分流无关(调整后的风险比,1.3;95% CI,0.45-3.9)。
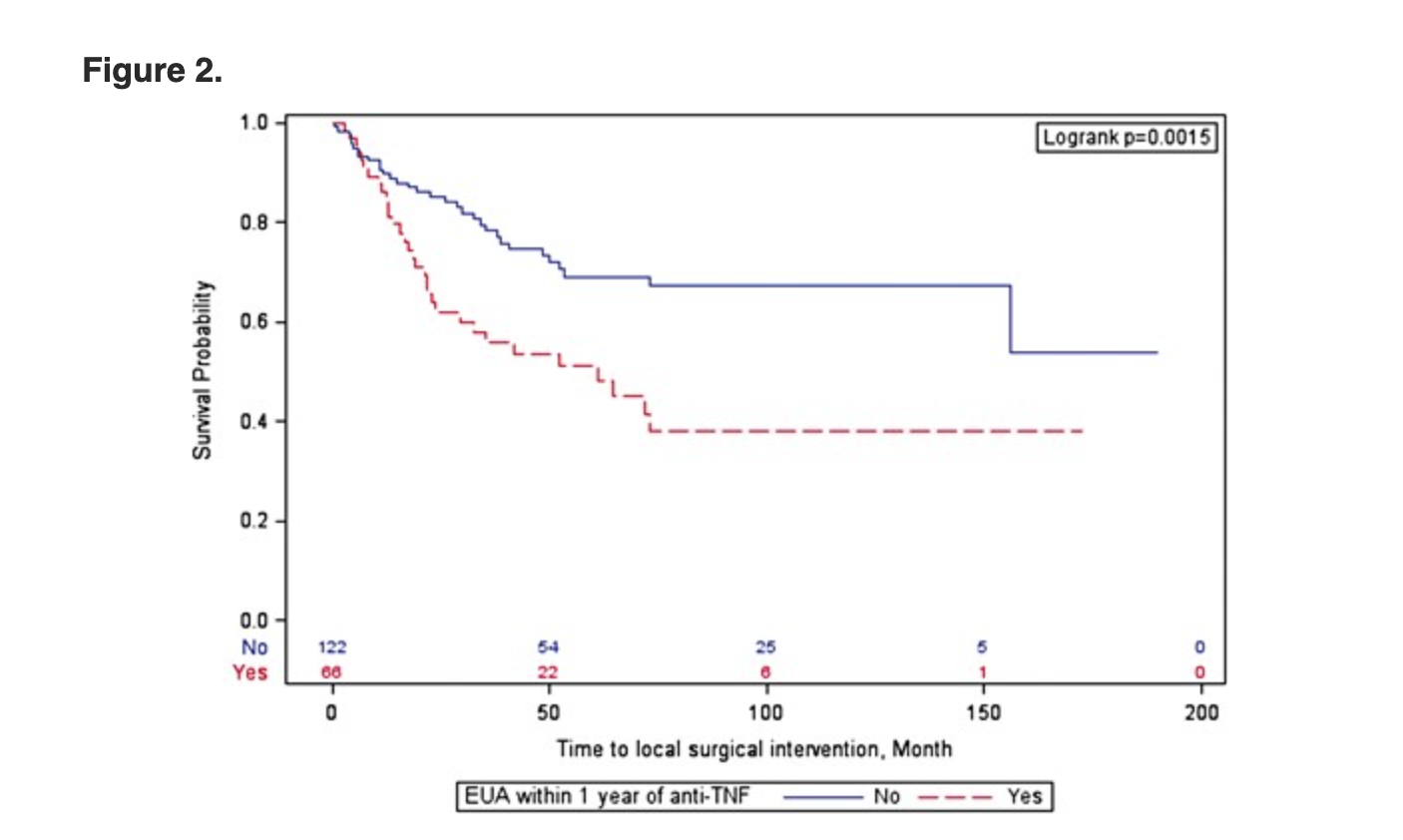
本项研究证实与单独的抗TNF治疗相比,抗TNF治疗前的EUA与改善临床结果无关,这表明EUA可能不是普遍需要的。但是未来控制瘘管严重程度的前瞻性研究是必要的。
原始出处:
Melissa Chan. Et al. Examination Under Anesthesia May Not Be Universally Required Prior to Anti-TNF Therapy in Perianal Crohn’s Disease: A Comparative Cohort Study. Inflammatory Bowel Diseases.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#抗TNF#
60
#抗TNF治疗#
54
#IBD#
111
#TNF#
41
学习了
49