Lancet haemat:深静脉血栓形成后,标准弹性加压治疗持续时间其实没必要那么长
2018-10-10 MedSci MedSci原创
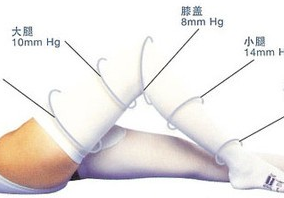
IDEAL DVT研究表明深静脉血栓形成后,在个体化基础上缩短弹性压迫的持续时间,对于预防血栓后综合征是安全的。现研究人员对该策略的成本效益进行评估。IDEAL DVT是一个多中心的随机化非非劣效性试验,招募腿部近端急性深静脉血栓形成的患者。经过6个月的弹性压迫治疗后,患者被随机(1:1)分至标准组(弹性袜加压2年)或缩短组(根据患者的Villalta评分缩短压迫持续时间)。同时评估患者的质量校正
IDEAL DVT是一个多中心的随机化非非劣效性试验,招募腿部近端急性深静脉血栓形成的患者。经过6个月的弹性压迫治疗后,患者被随机(1:1)分至标准组(弹性袜加压2年)或缩短组(根据患者的Villalta评分缩短压迫持续时间)。同时评估患者的质量校正的生活年(QALYs:以EQ-5D-3L和SF-36评估)和花费(€)。分别于确诊血栓形成后第3、6、12和24个月采集数据。以QALY阈值€30000计算净货币增殖效益。
2011年3月22日-2015年7月1日,共招募了865位患者,437位分至缩短组、428位分至标准组。9位患者因6个月内复发静脉血栓被排除研究。从社会角度来看,根据EQ-5D,每QALY损失,花费节约€305.992(净货币增殖效益€3205,95% CI 502–5741);根据SF-6D,每QALY损伤,花费节约€6030.941(€3540,95% CI 1174–5953)。采用EQ-5D的UK税收表,个体化疗法更为有效,且花费更少(€4071,1452–6647)。阈值为每QALY€30000时,个体化疗法是合理的的概率可达到99%。
与标准压迫疗法相比,个体化缩短弹性压迫治疗的持续时间是划算的。在深静脉血栓形成后,采用个体化方法挑战压迫治疗时间来预防血栓形成后综合征可在不降低健康相关的生活质量的前提下促进降低医疗成本。
Elham E Amin,et al. Individually shortened duration versus standard duration of elastic compression therapy for prevention of post-thrombotic syndrome: a cost-effectiveness analysis. The Lancet Haematology. October 09,2018.https://doi.org/10.1016/S2352-3026(18)30151-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉#
30
#静脉血#
30
#Lancet#
29
#HAE#
27
#EMA#
33
#静脉血栓形成#
33
#持续时间#
26
谢谢分享,学习了。
53