Nat Cell Biol:增加脂肪细胞竟能抗癌!
2017-11-09 佚名 MedSci原创
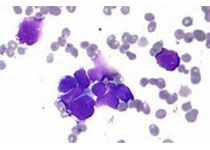
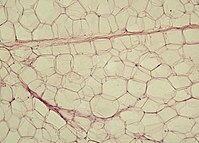
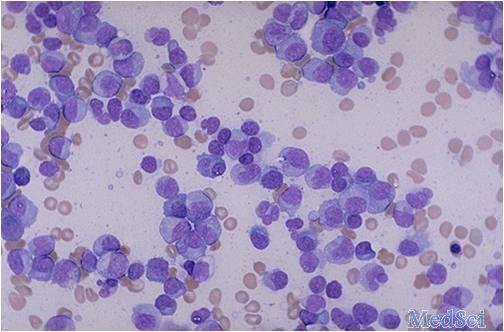
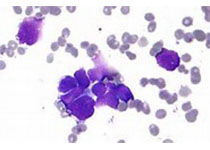
近日,来自加拿大 McMaster 大学干细胞与癌症研究所 Mickie Bhatia 教授所领导的研究团队发现,红骨髓(具有造血功能的骨髓,后面简称骨髓,虽然人体内也有富含脂肪细胞的黄骨髓,但是这里面的脂肪细胞不乐意帮红骨髓)中的脂肪细胞是人类骨髓中健康血细胞发育成熟所必须的。急性髓性白血病引发的机体造血功能障碍,就是通过抑制骨髓脂肪细胞生成实现的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CEL#
33
#Nat#
35
#Cell#
29
#Biol#
31
#Bio#
28
#脂肪细胞#
26