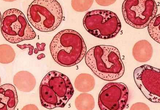
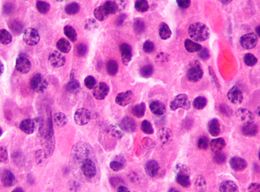
Lancet Oncol:多发性骨髓瘤——治疗方案怎么选?
2015-11-17 zhaozhou 译 MedSci原创
相对于接受传统化疗的近期被诊断为多发性骨髓瘤的患者,高剂量美法仑和自体干细胞移植(ASCT)可以延长无进展生存时间和总生存时间。这一策略目前也是治疗年龄65岁以下可以适用高剂量疗法的患者的标准方案。免疫调节药物(如沙利度胺和来那度胺)和蛋白酶体抑制剂(如硼替佐米)可以显著改善适合和不适合移植的患者的生存率。 澳大利亚的研究团队开展了一项多中心、非盲、三期临床试验,以比较化疗(环磷酰胺和地
相对于接受传统化疗的近期被诊断为多发性骨髓瘤的患者,高剂量美法仑和自体干细胞移植(ASCT)可以延长无进展生存时间和总生存时间。这一策略目前也是治疗年龄65岁以下可以适用高剂量疗法的患者的标准方案。免疫调节药物(如沙利度胺和来那度胺)和蛋白酶体抑制剂(如硼替佐米)可以显著改善适合和不适合移植的患者的生存率。
原始出处:
Francesca Gay et al. Chemotherapy plus lenalidomide versus autologous transplantation, followed by lenalidomide plus prednisone versus lenalidomide maintenance, in patients with multiple myeloma: a randomised, multicentre, phase 3 trial.The Lancet Oncology. Available online 17 November 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
39
#多发性#
26
#Lancet#
24
#治疗方案#
30