J Am Coll Cardiol:采用连续热稀释法测定冠脉疾病患者的**冠脉血流量
2021-03-04 MedSci原创 MedSci原创
冠状动脉内连续热稀释法是一种量化冠状动脉绝对血流量(Q)和阻力(R)的新技术
冠状动脉内连续热稀释法是一种量化冠状动脉绝对血流量(Q)和阻力(R)的新技术,与冠状动脉血流储备(CFR)和微血管阻力指数(IMR)等现有方法相比具有潜在的优势。然而,目前还没有关于缺血性和非梗阻性冠状动脉疾病(INOCA)患者的相关数据。
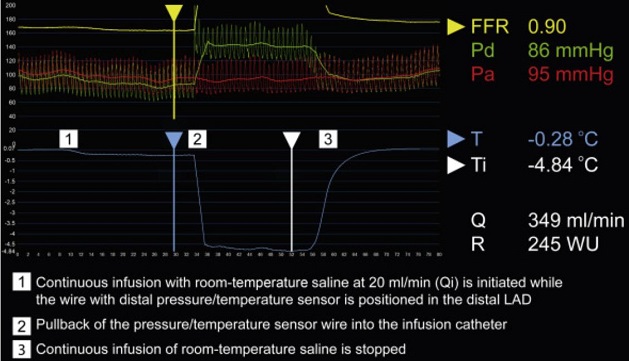
连续热稀释法检测示例
本研究旨在评估INOCA患者连续热稀释法检测的Q和R与已建立的CFR/IMR的关系,探讨Q绝对值的潜力,并预测自报性心绞痛。
共纳入了84例INOCA患者(87%女性,平均年龄56±8岁),予以冠状动脉功能检测,包括乙酰胆碱(ACH)激发试验、腺苷(ADE)试验(CFR/IMR)和连续热稀释(绝对值Q和R)伴盐水诱导性充血。
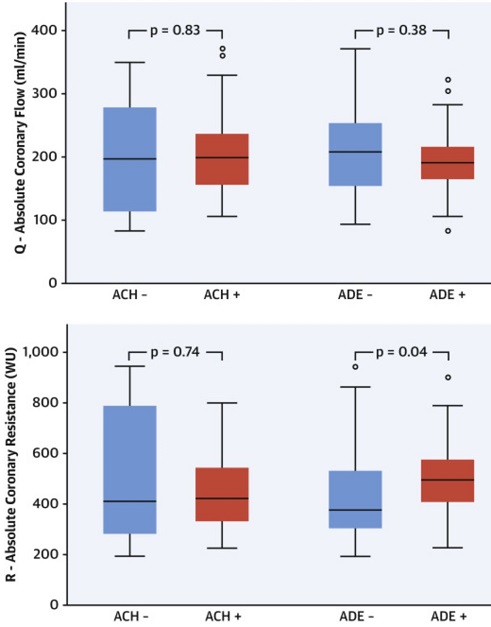
根据ACH和ADE检测的绝对冠脉血流和阻力
ACH检测的异常率为87%,ADE检测的异常率为38%。Q的绝对中位值为198ml/min,R的绝对中位值为416WU。ADE检测异常的患者的绝对R值高于ADE检测正常的患者(495WU vs 375WU;P=0.04),但ACH检测异常和ACH检测正常的患者之间没有差异(421WU vs 409WU;P=0.74)。
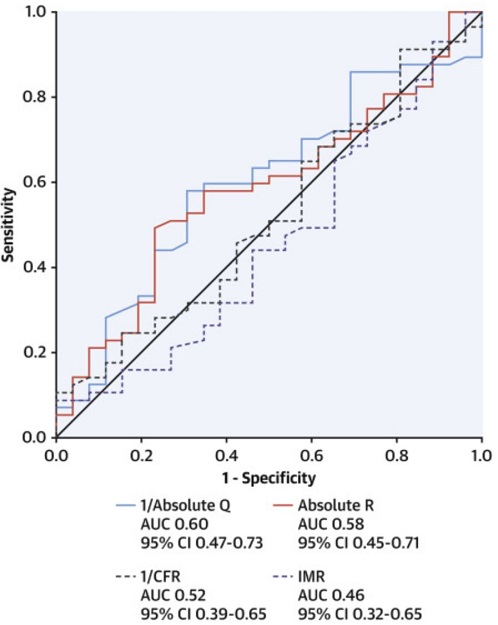
Q、R、CFR和IMR对心绞痛的预测价值
低Q和高R值均与严重心绞痛相关(优势比[OR]分别为:3.09,95%CI 1.16~8.28,P=0.03;和2.60,0.99~6.81,P=0.05)。
在本研究中,CFR/IMR异常的患者的R绝对值较高,但Q和R与冠状动脉血管痉挛均无关。Q和R与心绞痛相关,不过它们的确切预测价值还应该在更大的研究中进一步确定。
原始出处:
Konst Regina E,Elias-Smale Suzette E,Pellegrini Dario et al. Absolute Coronary Blood Flow Measured by Continuous Thermodilution in Patients With Ischemia and Nonobstructive Disease. J Am Coll Cardiol, 2021, 77: 728-741.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血流量#
40
#Cardiol#
36
#疾病患者#
37
#Coll#
30
#测定#
39
#热稀释法#
24
#冠脉疾病#
50