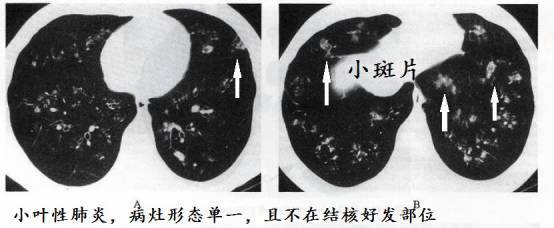
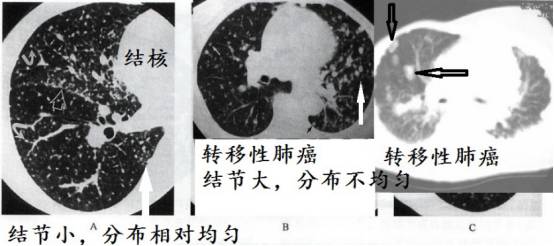
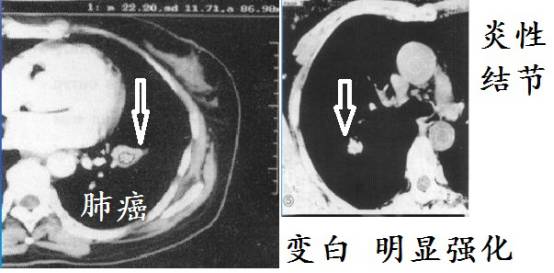
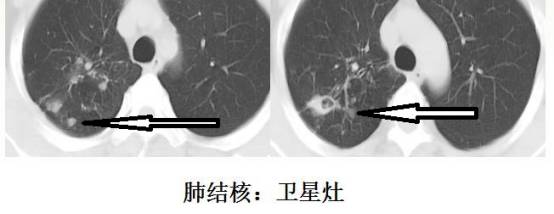
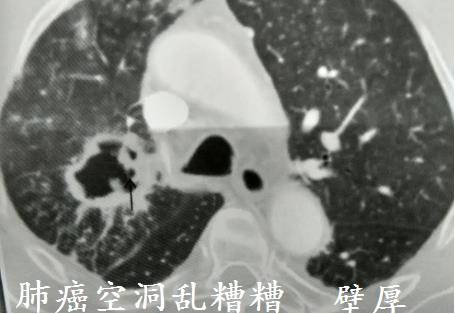
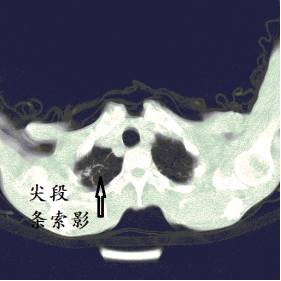
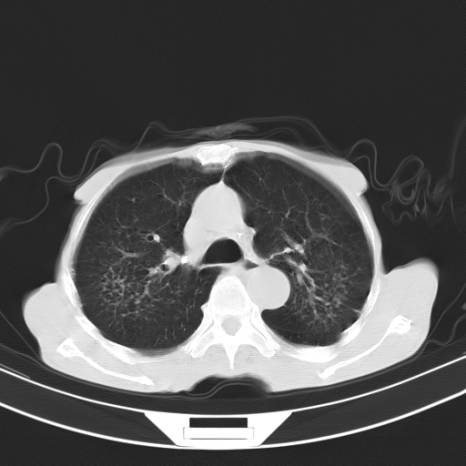
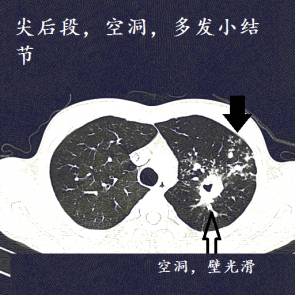
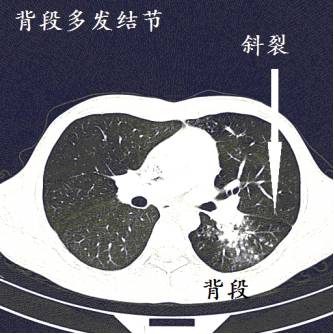
为什么经验丰富的医生一看CT就知道是肺结核?因为肺结核的CT很有特点! 1、好发部位 肺结核好发于上叶的尖后段和下叶的背段,这是肺结核最基本的特点! 为什么结核容易长在这些地方,目前没有公认的理由。 可能因为人直立时,这些部位的血压相对低, 血液循环差,巨噬细胞减少,导致局部抵抗力低。并且,这些部位氧气多,结核是需氧菌,在上叶的尖后段和下叶的背段聚集,正所谓占尽天时地利。 2、病灶多形态 很多结核,特别是典型的肺结核,往往是很多种形态。大叶性肺炎,表现为斑片状阴影;肺癌,表现为肿块,或者结节;金葡菌肺炎,常出现空洞。 但是,肺结核常常有条索状阴影,有大小不等的结节,有空洞,有实变,有大小不等的斑片状阴影等,多种形态的病灶混合在一起! 下图是普通细菌引起的小叶性肺炎,病灶形态单一。 3、多部位 早期肿瘤、大叶性肺炎等,常常局限在某一个肺叶生长。但是,肺结核的本质就像资本主义,喜欢到处扩张地盘,就像美国,恨不得这个太阳系都是他家的!很多典型的肺结核常常侵犯多个肺叶或者肺段! 4、常有结节 肺结核,其中“结”字,反映在CT上就是常常有大小不等的多发结节!个人发现,肺结核的CT很少没有结节的!如上图。 并且,肺结核多发的结节,一般偏小。假如结节偏大,分布不均匀,则要考虑转移性肺癌。 5、结节一般不会堆积在一起 肺结核的光棍特征,肺结核虽然子满天下,但是不像肿瘤喜欢同性恋(多个结节堆积在一起),肺结核的小结节常常分散在两肺,各玩各的,各自为政! 6、少肿块 肺结核很少形成肿块!假如一个肿块,肺穿刺活检提示肉芽肿,也不要轻易诊断肺结核,而要考虑肺癌。 以前遇到一个病人,一大个肿块,穿刺病理肉芽肿,再次穿刺:肺癌。除非病理报干酪性坏死,要不然,肿块不要轻易诊断肺结核,那是肺癌的特色。 肺结核因为干酪性坏死,增强CT强化一般不明显!但是,有些肺结核在增殖阶段,生长活跃,没有形成明显坏死,有可能显著增强。 这个要综合考虑。但是大多数肺结核增强一般不会显著强化。肺癌生长需要血供,常常显著强化。 无强化:强化CT值<10Hu;轻度强化:强化CT值达10~20Hu;中度强化:强化CT值达20~30Hu;重度强化:强化CT值≥30Hu。 也有学者这样分类:轻度强化:CT值上升<20HU;中度强化(CT值上升20~40HU),明显强化(CT值上升>40HU)。 简单的说,就是增强CT上,病灶越白,强化也明显,肿瘤、一般细菌感染引起炎性结节常常明显强化,肺结核强化不明显。 上图是肺结核增强CT,病灶几乎无强化,和下面差别很大。 肺结核生长缓慢,容易形成钙化!虽然很多疾病,包括肺癌也会钙化,但是肺结核钙化相对更常见! 传统的方法培养结核菌需要多久?大约2月!结核杆菌生长缓慢,肺结核一般病灶变化也很慢! 一般细菌如同撒尿,来也匆匆,去也匆匆!肺结核是瘟神,老年性痴呆!来也慢吞吞,去也慢腾腾。假如抗感染治疗,三五天病灶就吸收了大半,那几乎可以排除肺结核。 肺结核的结节常常多发,不喜欢堆积,就算是一个结节,也要整个卫星病灶。就像官僚主义,出行总要带个卫兵,要不然没有面子! 肺结核喜欢在光滑的地板上摩擦!肺结核的空洞壁常很光滑,典型的光滑且壁薄。肺癌空洞则壁厚,且乱糟糟的。 毁损肺,就是肺废掉了,肺烂掉、几乎没有功能了。在中国等等非发达国家,毁损肺大多数是肺结核造成的。结核毁一生。 摄影穷三代,单反毁一生!考古穷三代,盗墓毁一生。甚至还有人说:清华毁一生,北大穷三代。来来来,你来读云南大学,让我来读北大穷三代。 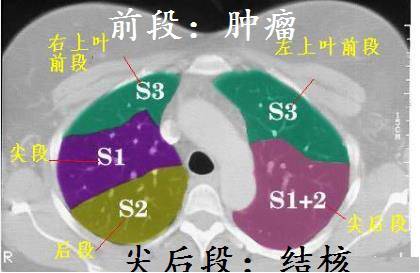

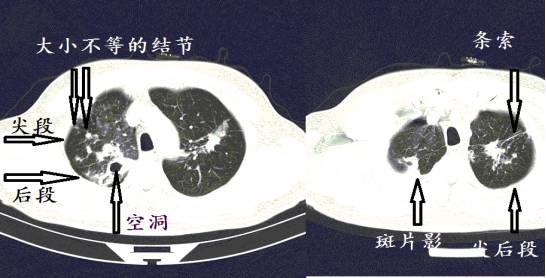
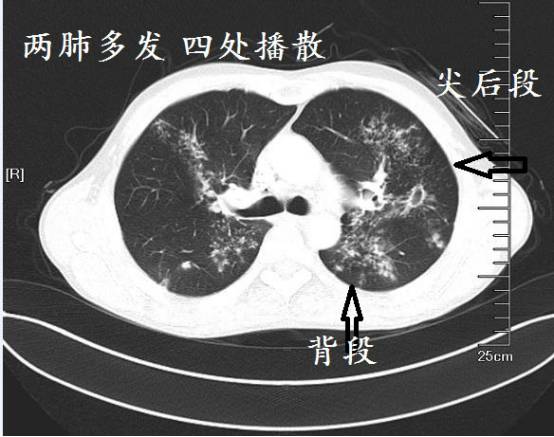



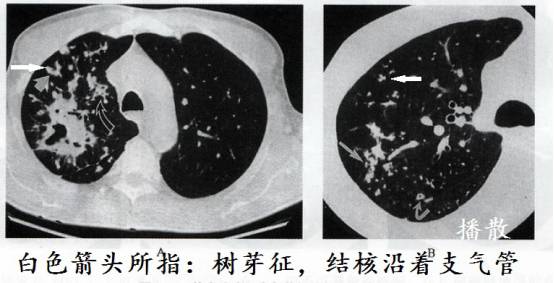
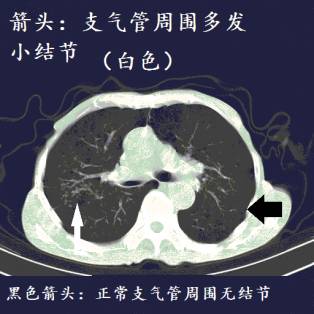
结核的特点之一便是沿着支气管播散,在支气管周围形成密密麻麻的小结节,在外周小支气管播散形成树芽征。虽然其他疾病也会这样,但是结核相对更常见。

所谓结核沿着支气管播散,简单的说就是病灶大部分都分布在支气管周围。
下图是我在肺部影像联盟看到的一个特殊空洞,支气管进入空洞,提示结核,我把它也理解为结核沿着支气管播散的一个情况。

下面,再举例十二个病人的肺CT图像详细解读!


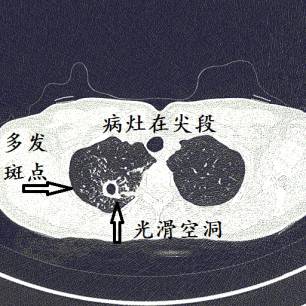
结核,为什么?
1.病灶在结核好发部位(尖后段、背段);
2.病灶形态多样,有空洞,有小结节,有斑片影;
3.空洞壁光滑;
4.病灶分布广,上叶尖后段、下叶背段都有;
5.增强CT,病灶无明显强化。
结果:抗酸杆菌阳性,抗结核治疗病情好转。
纵膈窗提示钙化
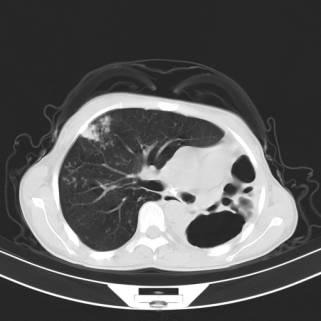
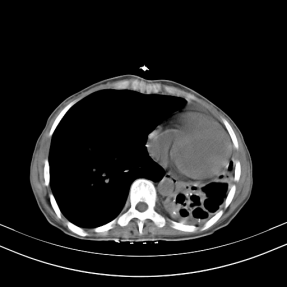
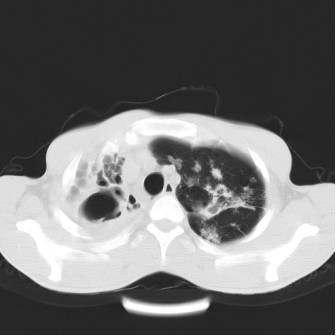
结核,为什么?
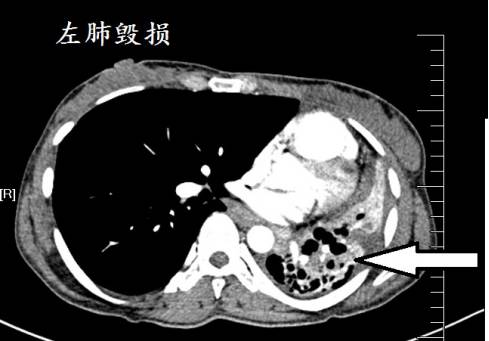
1.左肺:毁损肺;
2.右肺病灶在结核好发部位(尖后段);
3.有小结节,且沿着支气管播散;
4.有钙化。
结果:抗酸杆菌阳性,抗结核治疗,症状好转。毁损肺,依旧毁损。
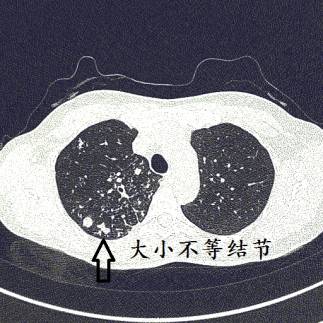

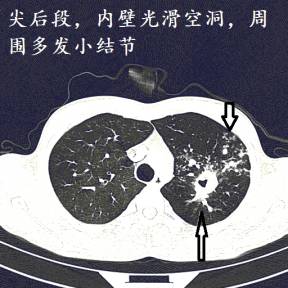
结核,为什么?
1.病灶在结核好发部位(尖后段、背段);
2.病灶形态多样,有空洞,有小结节,有实变;
3.空洞壁光滑;
4.病灶分布广,上叶、下叶背段都有。
结果:抗酸杆菌阳性,抗结核治疗病情好转。

结核可能性很大,为什么?
1.病灶在结核好发部位(尖后段);
2.病灶形态多样,有条索影,有小结节;
3.小结节沿着支气管播散;
4.病灶分布广,左肺右肺都有。
结果:抗酸杆菌阳性,抗结核治疗病情好转。

增强CT:强化不明显,有钙化
结核可能性很大,为什么?
1.病灶在结核好发部位(尖后段、背段);
2.病灶形态多样,有空洞,有小结节,有斑片影;
3.空洞壁光滑;
4.病灶分布广,上叶尖后段、下叶背段都有;
5.增强CT,病灶无明显强化;
6.空洞有钙化。
结果:抗酸杆菌阳性,抗结核治疗病情好转。
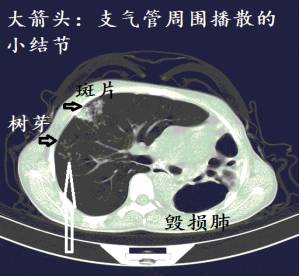
空洞,多发结节影
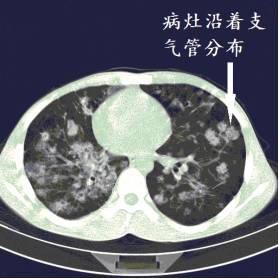
病灶多发,沿着支气管分布
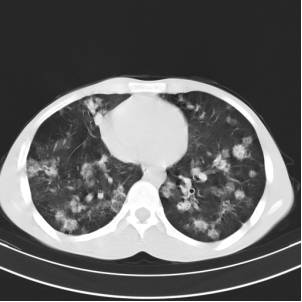
病灶多发,像满天烟花
结核可能性很大,为什么?
1.病灶双肺多发;
2.病灶形态多样,有空洞,有结节影;
3.部分病灶很明显的沿着支气管播散。
结果:抗酸杆菌阳性,抗结核治疗病情好转。
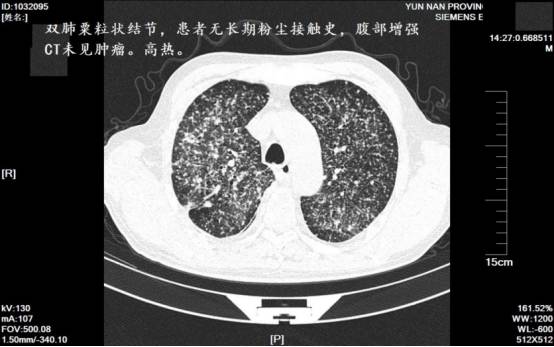
结核可能性很大,为什么?
1.双肺粟粒状结节,分布均匀,结节小;
2.未见肿块;
3.无粉尘接触史,基本排除尘肺;
4.无明显其他器官癌症依据,转移性肺癌可能性不大;
5.高热,支持感染性疾病。
结果:抗结核治疗病情好转。
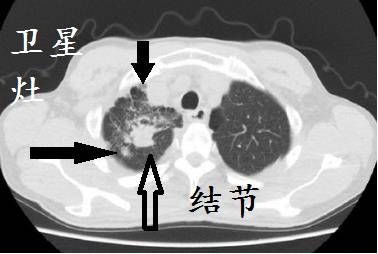
结核,为什么?
尖段结节,周围卫星病灶。

淋巴结结核,为什么?
结核中心干酪样坏死,不强化,外周强化,形成环形强化。
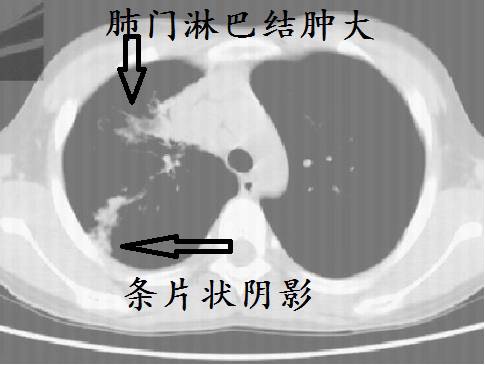
假如这个是儿童的CT,则诊断什么?
肺结核,原发综合征。
为什么?
因为儿童的肺结核,常表现为斑片状阴影,同时伴有肺门淋巴结肿大,在胸片上表现为哑铃状。


假如上图是年轻人,考虑什么?
在中国等非发达国家,结核很常见。
假如年轻人,单侧胸腔积液,没有肺炎,一般都是结核。
假如胸水为渗出液,ADA升高,则几乎都是结核性胸膜炎。
结核球病例的文献,图太难看。再来一个我管过的病人。
患者30岁,既往患“胸膜炎”,具体不详。胸痛1月,其余正常。

首选按普通感染治疗,抗感染治疗2周,病灶无明显好转。肺穿刺:肉芽肿。抗结核治疗2月,完全吸收。妥妥的结核球。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












喜欢这种学习方式。顶!
36
学习到很多,感谢分享。
69
#结核#
45
学到了
65
学习了
0
实了取栓治疗在前循环大血管闭塞性
0
好文章,谢谢分享。
44