Dev Cell:垂死的细胞保护它们的邻居以保持组织的完整性
2021-07-12 Viho MedSci原创
为了使组织更新,人类组织不断地消除数以百万计的细胞,而不损害组织的完整性、形态和连接性。维持这种完整性所涉及的机制仍然是未知的。
为了使组织更新,人类组织不断地消除数以百万计的细胞,而不损害组织的完整性、形态和连接性。维持这种完整性所涉及的机制仍然是未知的。
来自巴斯德研究所和法国国家科学研究中心的科学家们今天揭示了一个新的过程,它允许被淘汰的细胞暂时保护其邻近的细胞死亡,从而保持组织的完整性。这种保护机制是至关重要的,如果被破坏,会导致暂时失去连接。科学家们观察到,当该机制被停用时,几个相邻的细胞同时被消除会损害组织的完整性。这种完整性的缺乏可能是导致慢性炎症的原因。这项研究的结果发表在Developmental Cell杂志上。

人类上皮细胞是在身体的几个部位发现的组织(如表皮和内部粘膜)。它们由连续的细胞层组成,起到物理和化学屏障的作用。这一作用不断受到外界环境和自身更新的考验。组织更新包括通过细胞分裂形成新细胞和消除死亡细胞。这种情况在胚胎发育或成人组织的维护过程中经常发生,在涉及大量被淘汰的细胞的情况下,调节上皮细胞保持其完整性的能力的机制仍然不为人所知。
科学家们通过使用果蝇(或称醋蝇)来确定参与上皮完整性的机制以及能够影响上皮连接的条件,果蝇是一种在实验室中研究的生物,其上皮结构与人类相似。研究小组利用蛋白质敏感的荧光标记,发现当一个细胞死亡时,EGFR-ERK途径--一种因参与调节细胞生存而闻名的细胞激活信号途径--在邻近的细胞中被暂时激活。科学家们观察到,EGFR-ERK途径的激活保护了邻近的细胞免受细胞死亡的影响,时间大约为一小时,从而防止了一群细胞同时被消灭。这一途径在调节上皮组织的细胞存活方面起着关键作用,还能观察到细胞之间的这种保护性动态。
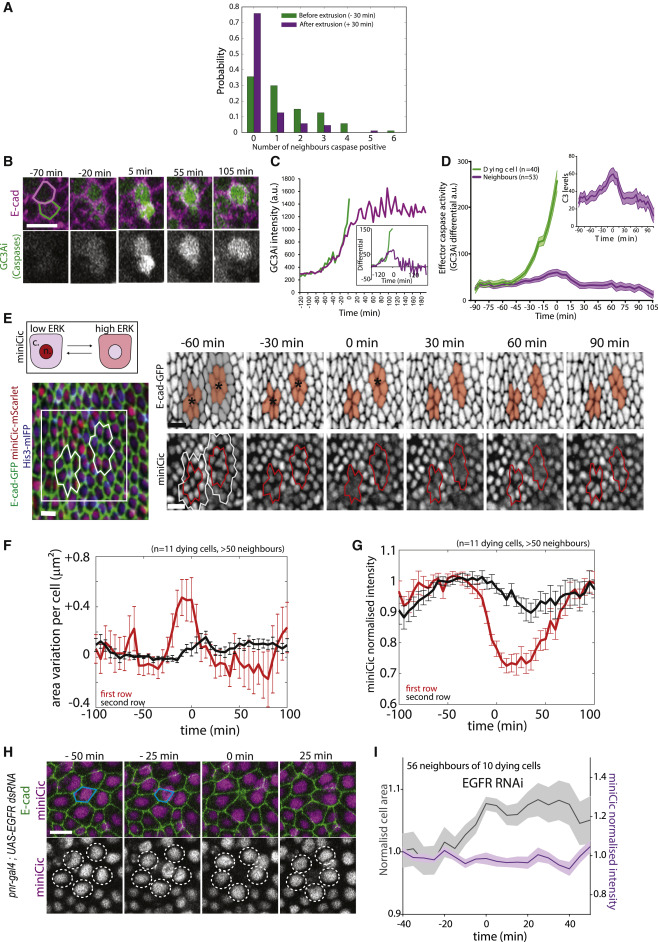
挤压细胞附近细胞的瞬时ERK激活
科学家们的研究还表明,抑制这种保护机制会对上皮组织产生剧烈的影响:细胞的消除变得随机,相邻的细胞可能同时被消除,导致连接性的反复丧失。在正常情况下,当EGFR-ERK途径没有被刻意抑制时,即使有大量的细胞被消除,也从未在上皮组织中观察到相邻细胞群的消除现象。
通过使用一种新的光遗传学工具,可以在时间和空间上控制细胞死亡,并绕过保护机制,科学家们证实,当相邻的细胞同时被消除时,上皮的完整性会受到损害。"令人惊讶的是,上皮组织对被淘汰细胞的空间分布高度敏感。虽然它可以承受大量细胞的消除,但如果只有三个相邻的细胞同时被消除,上皮的完整性就会受到影响。

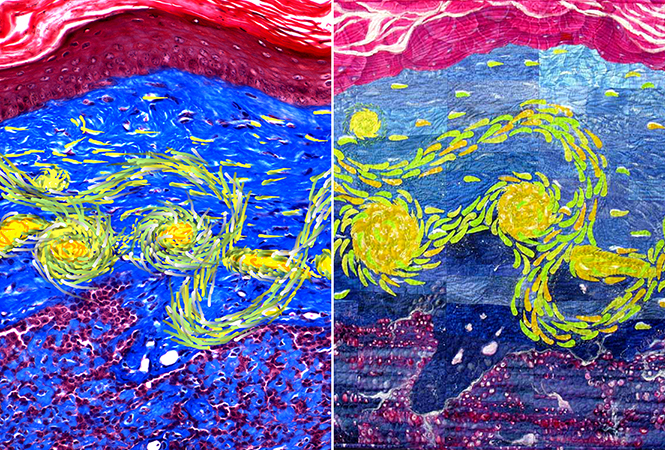
三个或更多细胞团的挤压足以破坏上皮的封闭
科学家们的观察证实,组织需要发展出防止相邻细胞群被淘汰的机制。这些观察结果很重要,因为它们说明了生物组织令人难以置信的自组织能力,这一特性使它们能够承受压力条件。不需要一个中心来协调细胞应该在哪里和何时死亡;一切都基于相邻细胞之间的高度局部通信。
这一过程似乎在进化过程中一直保持着。每一个细胞死亡附近发生的短暂和局部保护阶段。这种保护是由细胞内ERK的瞬时激活驱动的,ERK在邻近的挤压细胞中被激活,阻止细胞团簇的清除。
未来的研究将揭示这种细胞死亡协调机制的破坏和上皮组织中连接性的反复丧失是否可能是慢性炎症的根源之一,而慢性炎症是造成各种疾病的现象,目前是全球死亡的主要原因之一。
文章参考:Léo Valon, Anđela Davidović, Florence Levillayer, Alexis Villars, Mathilde Chouly, Fabiana Cerqueira-Campos, Romain Levayer.Robustness of epithelial sealing is an emerging property of local ERK feedback driven by cell elimination. Developmental Cell, 2021; 56 (12): 1700 DOI:10.1016/j.devcel.2021.05.006
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#Cell#
34
#完整性#
32
#Dev#
49
#CEL#
42
理学组织
64