JACC:经导管主动脉瓣置换后永久性起搏器植入的发生率及对预后的影响
2021-05-11 MedSci原创 MedSci原创
在当下大量的ViV-TAVR患者中,围手术期PPI的发生率相对较低,并且随着新一代THV系统的使用,其发生率进一步降低了
永久性心脏起搏器植入(PPI)仍然是经导管主动脉瓣置换术(TAVR)的主要缺点之一,但是瓣膜瓣(ViV)TAVR后发生PPI的数据很少,尤其是在使用新一代经导管心脏瓣膜(THV)的情况下的相关数据更少。
本研究目的是在一个大型ViV-TAVR项目中明确PPI的发生率、相关风险因素和对患者临床预后的影响。
研究人员从多中心VIVID注册处收集了相关数据,根据围手术期PPI的需要,主要分析了基线和手术特征,以及院内和晚期(中位随访13个月)预后。除CoreValve、Cribier-Edwards、Sapien和Sapien XT之外的所有THV均被视为新一代THV。
不同瓣膜之间的PPI发生率对比
共纳入了1987位于2007年至2020年期间接受ViV-TAVR的既往无PPI史的患者。其中,128位(6.4%)患者在TAVR后接受了PPI,使用新一代THV的患者的PPI发生率显著降低(4.7% vs 7.4%,p=0.017),最明显的是使用Evolut R/Pro的患者(Evolut R/Pro vs CoreValve:3.7% vs 9.0%,p=0.002)。新一代球囊和自扩张THV之间的PPI发生率无显著差异(6.1% vs 3.9%,p=0.18)。
PPI相关风险因素及对预后的影响
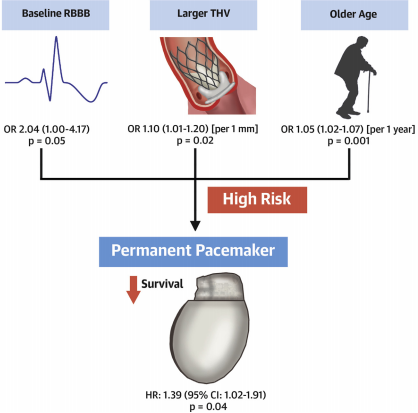
在多变量分析中,老年、THV尺寸较大和既往右束支传导阻滞均与PPI发生风险增加有关(优势比[OR]分别是:1.05/1年,p=0.001;1.10,p=0.02;2.04,p=0.05)。
不同分组的存活预后
PPI组和无PPI组的30天内死亡率无明显差异(4.7% vs 2.7%,p=0.19)。但在随访过程中,PPI患者表现出更高倾向的死亡风险(风险比 1.39,95%CI 1.002-1.91,p=0.04)。
总之,在当下大量的ViV-TAVR患者中,围手术期PPI的发生率相对较低,并且随着新一代THV系统的使用,其发生率进一步降低了。此外,ViV-TAVR后的PPI的发生与随访过程中死亡率增加的趋势有关。
原始出处:
Alperi Alberto,Rodés-Cabau Josep,Simonato Matheus et al. Permanent Pacemaker Implantation Following Valve-in-Valve Transcatheter Aortic Valve Replacement: VIVID Registry. J Am Coll Cardiol, 2021, 77: 2263-2273. https://doi.org/10.1016/j.jacc.2021.03.228
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#发生率#
32
#置换#
31
#JACC#
0
#永久性起搏器植入#
42
学习了
43
#起搏器#
38
#ACC#
20
#主动脉瓣#
25
#主动脉#
20
#经导管#
49