JAMA Oncology:循环肿瘤DNA有望预测结直肠癌的复发
2019-05-29 佚名 生物通
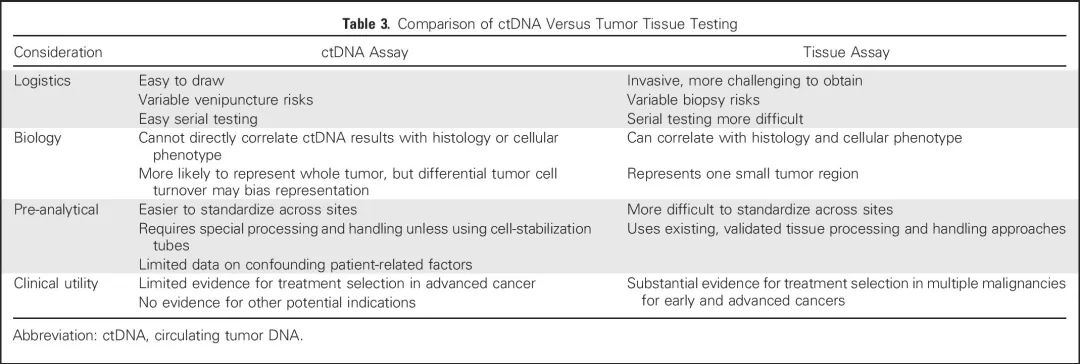
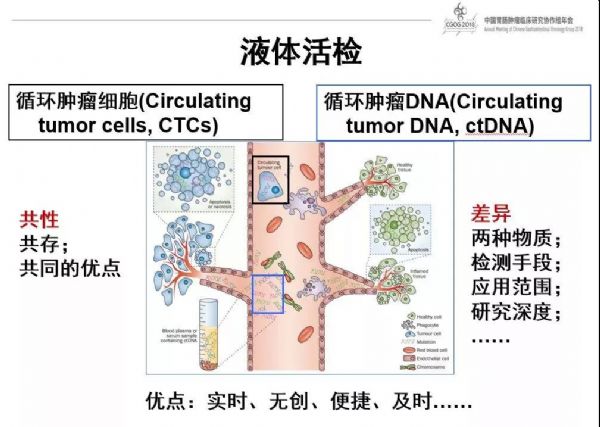
两个独立的研究团队近日发现,利用循环肿瘤DNA(ctDNA)可预测非转移性结直肠癌的预后和复发。这些研究成果于本周发表在《JAMA Oncology》杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
28
#Oncology#
30
好好好好好好
68
#结直肠#
30
#循环肿瘤DNA#
0
学习学习学习
63
谢谢了,学习
46