Sci Adv:方向前/王秀梅开发水凝胶递送miRNA策略,通过抗衰老治疗骨关节炎
2022-04-16 “生物世界”公众号 “生物世界”公众号
持续的miR-29b-5p递送和干细胞的募集以及随后分化成软骨细胞实现了成功的软骨修复和软骨细胞再生。该研究表明基于miRNA的治疗方式替代传统手术治疗骨关节炎具有巨大潜力。
骨关节炎(Osteoarthritis,OA)是一种常见的退化性疾病,导致关节软骨不可逆转的丧失。骨关节炎的病因很复杂,涉及到许多因素,包括遗传、急性损伤和慢性炎症。据公开资料显示,2018年我国关节炎患者已达到1亿人。但目前临床上缺乏有效的治疗方法。
近日,浙江大学医学院附属邵逸夫医院方向前团队和清华大学材料学院王秀梅团队合作,在 Science Advances 期刊在线发表题为:Stem cell-homing hydrogel-based miR-29b-5p delivery promotes cartilage regeneration by suppressing senescence in an osteoarthritis rat model(基于干细胞归巢水凝胶的miR-29b-5p递送通过抑制衰老促进软骨再生)的研究论文。
该研究提出了通过抑制骨关节衰老促进软骨再生治疗骨关节炎(OA)的新策略,通过生物材料构建抑制衰老的再生微环境来使因OA受损的软骨恢复活力。首次发现并验证了OA软骨衰老相关的miRNA——miR-29b-5p,并通过原位注射具有干细胞归巢活性的自组装多肽纳米纤维水凝胶缓释递送miR-29b-5p,同时募集内源性滑膜间充质干细胞(SMSCs)。
持续的miR-29b-5p递送和干细胞的募集以及随后分化成软骨细胞实现了成功的软骨修复和软骨细胞再生。该研究表明基于miRNA的治疗方式替代传统手术治疗骨关节炎具有巨大潜力。
OA的典型特征是软骨进行性丧失和润滑滑液减少,OA发展过程中软骨细胞衰老会导致软骨分解。研究团队首次证明了miR-29b-5p在OA软骨中显着下调,其上调通过易位酶1(TET1)抑制基质金属蛋白酶和衰老相关基因(P16INK4a/P21)的表达,有效缓解OA关节软骨的现状,延缓衰老进程。
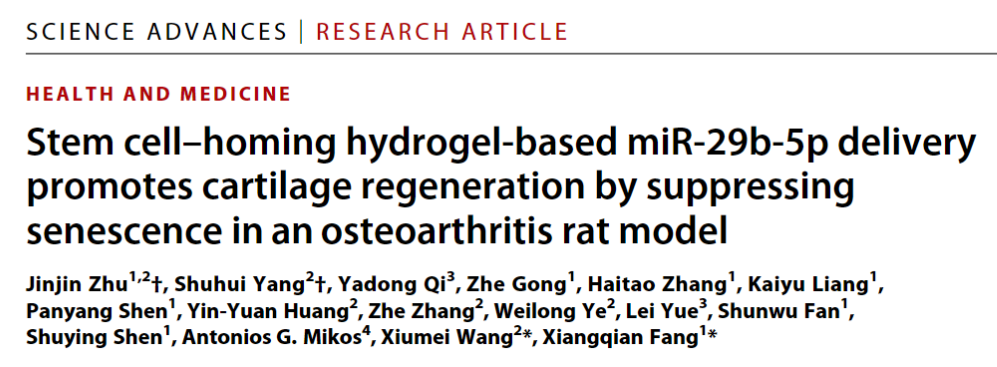
随后,团队开发了基于干细胞归巢水凝胶的miRNA递送系统SKP@miR(图1)。一方面,miR-29b-5p的持续递送能够抑制软骨细胞衰老,改善OA关节中软骨基质合成和分解之间的不平衡,从而抑制OA对软骨基质的持续性破坏;另一方面,SKP@miR招募SMSCs,并诱导其向软骨细胞分化,给受损基质补充健康软骨细胞,以修复缺陷并形成新的软骨,且无需使用外源性干细胞。
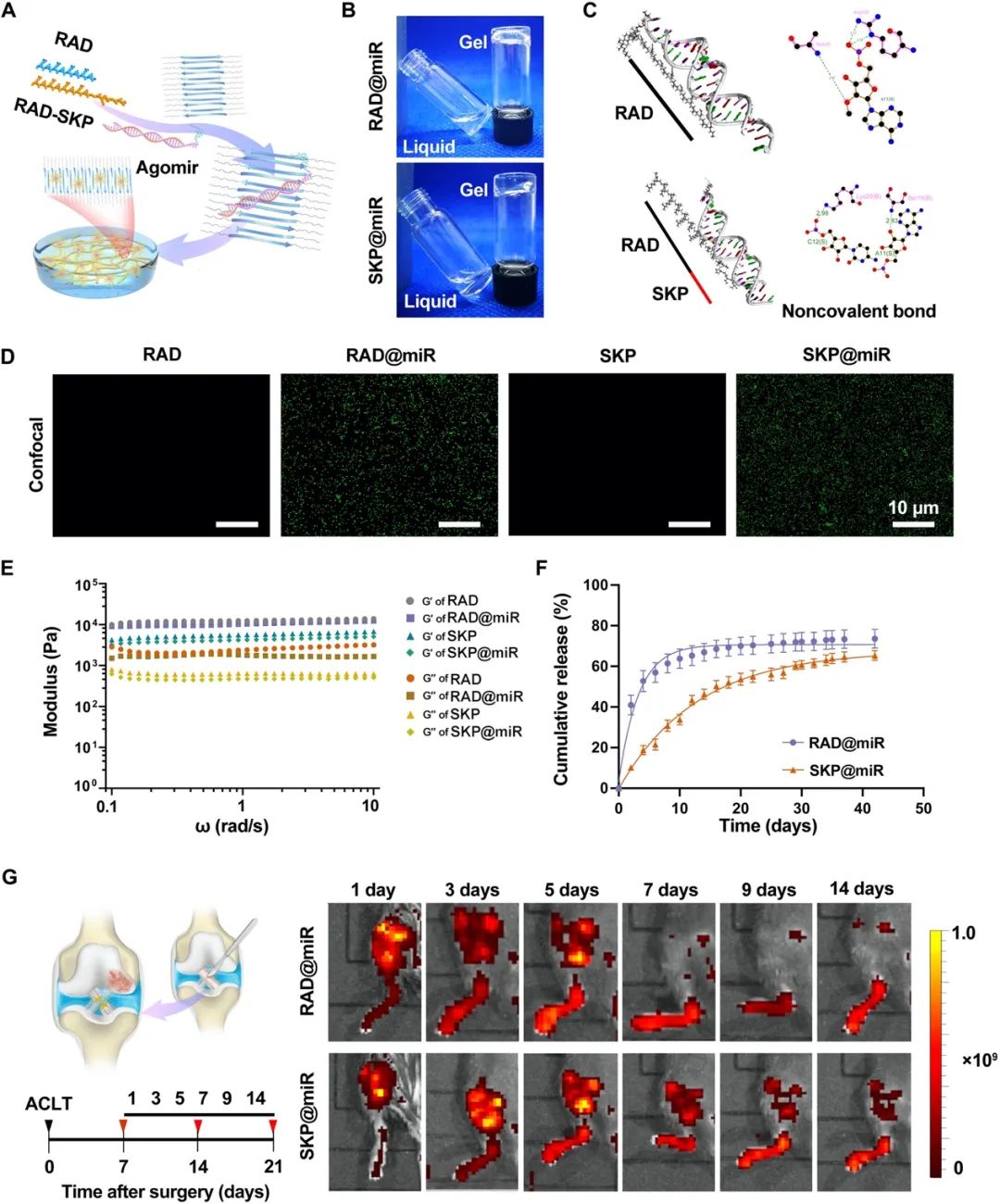
图1.基于水凝胶的miR-29b-5p递送系统SKP@miR的构建。(A)RAD和RAD-SKP多肽自组装形成纳米纤维水凝胶,agomir-29b-5p分布在水凝胶内部。(B)通过调节pH值至中性形成稳定的水凝胶。
研究表明,SKP@miR能够抑制OA大鼠关节软骨细胞的衰老和软骨基质的分解,促进软骨基质的合成,改善关节磨损,最终使受损关节恢复到与正常关节相似的状态(图2)。
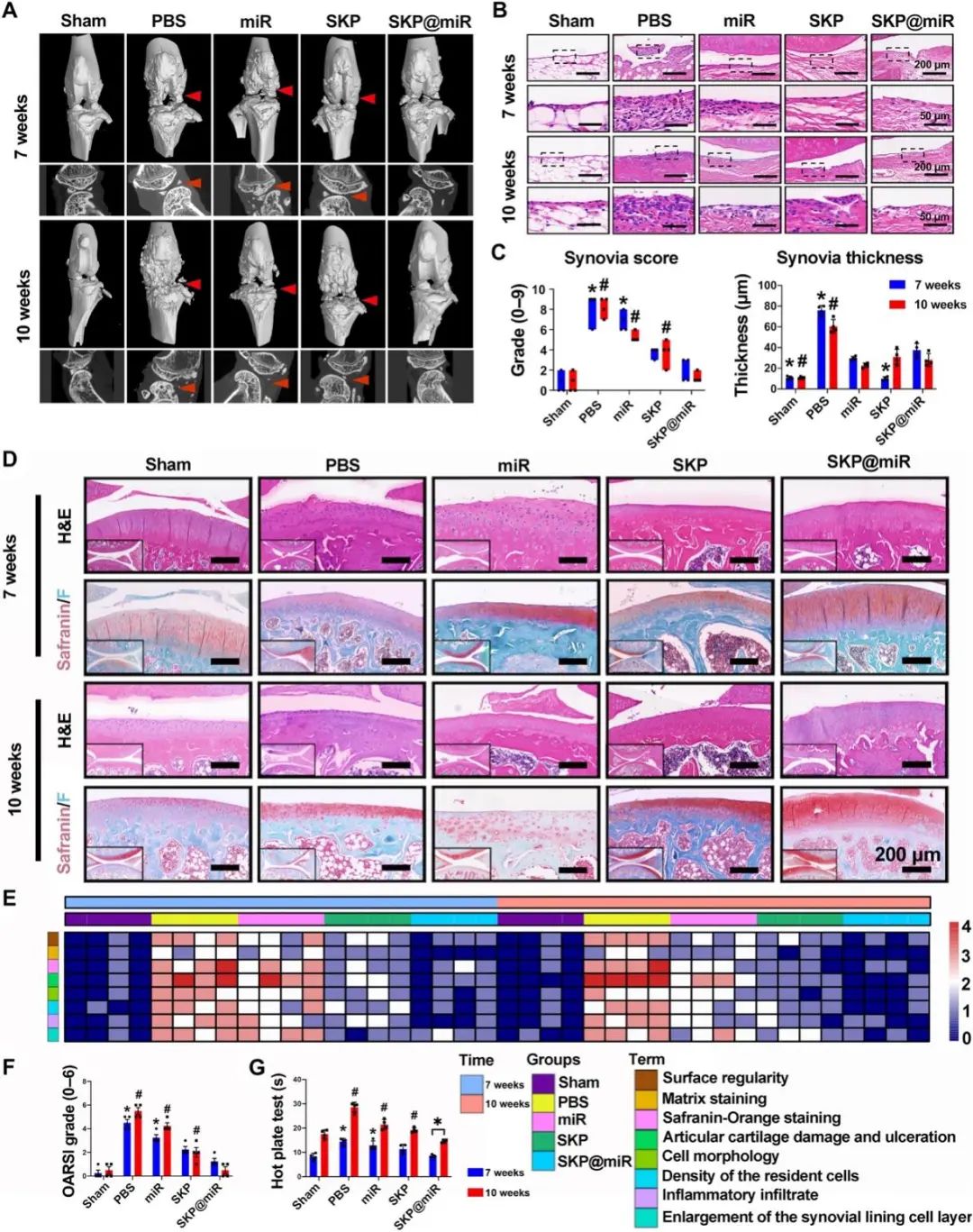
图2. SKP@miR递送miRNA显着减弱大鼠关节衰老
总的来说,该研究利用可注射水凝胶递送miRNA通过抗衰老治疗OA的策略效果显着,在临床应用中更方便实用,这对于开发针对OA的疾病修饰疗法具有重要意义。
浙江大学医学院附属邵逸夫医院诸进晋博士、清华大学材料学院杨淑慧博士为本论文共同第一作者,清华大学材料学院王秀梅研究员、浙江大学医学院附属邵逸夫医院方向前教授为共同通讯作者。合作者包括美国莱斯大学Antonios G. Mikos院士等,该研究还得到了浙江大学医学院附属邵逸夫医院骨科主任范顺武教授的指导。
原始出处:
JINJIN ZHU, et al. Stem cell–homing hydrogel-based miR-29b-5p delivery promotes cartilage regeneration by suppressing senescence in an osteoarthritis rat model. SCIENCE ADVANCES, 30 Mar 2022, Vol 8, Issue 13.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#miR#
40
#骨关节#
53
#关节炎#
41
#水凝胶#
52
#miRNA#
37
#凝胶#
46