60多张PPT搞定静脉溶栓并发症的预防和处理!
2021-11-04 郑州市中心医院 郑州市中心医院
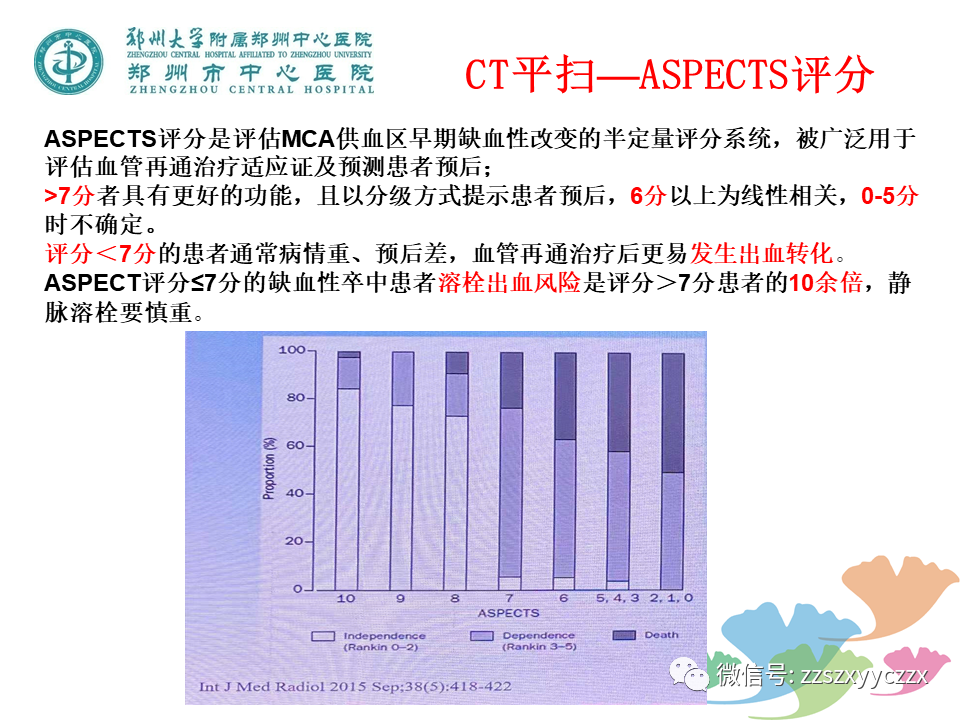
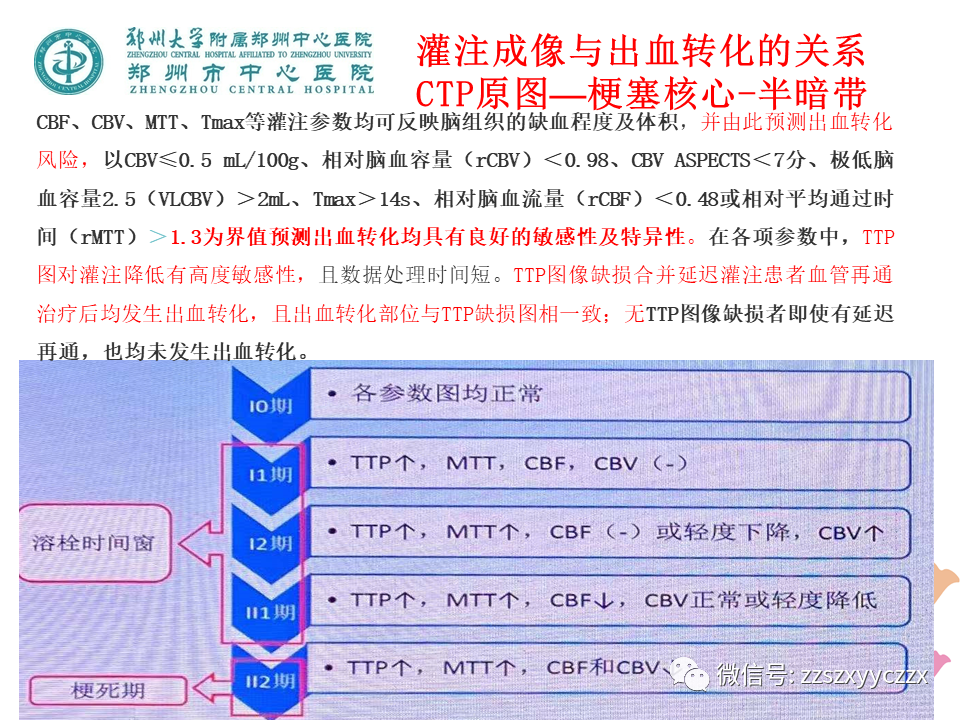
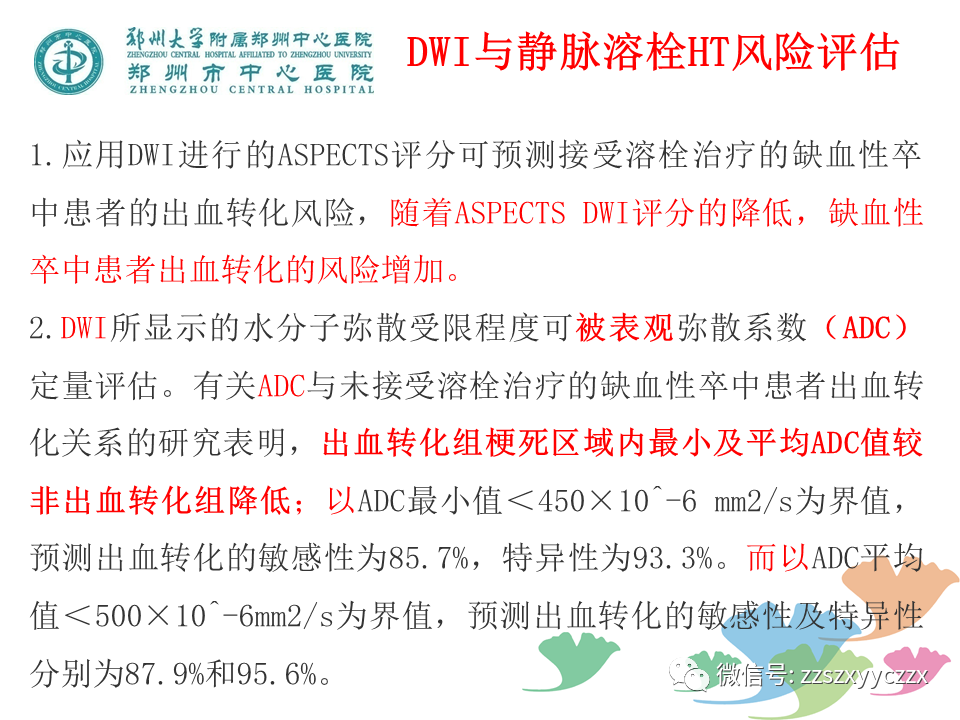
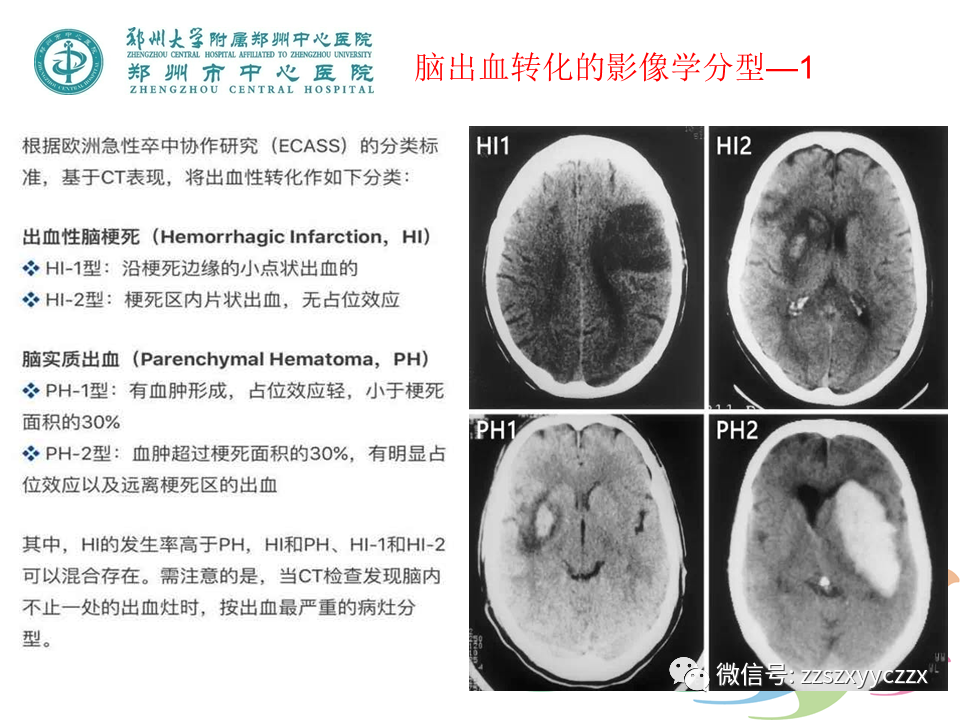
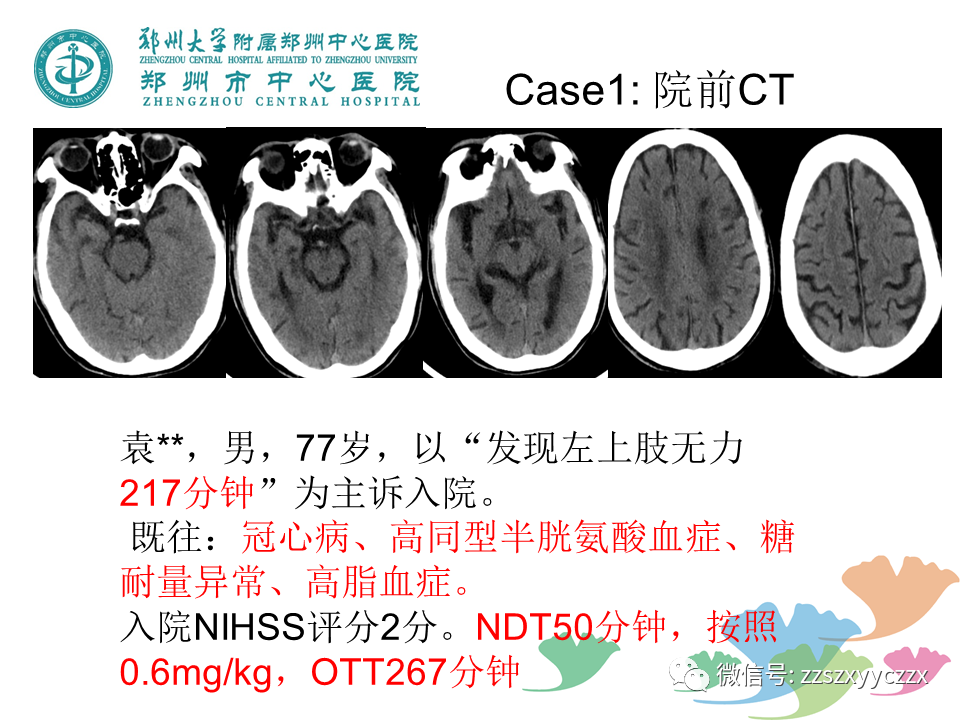
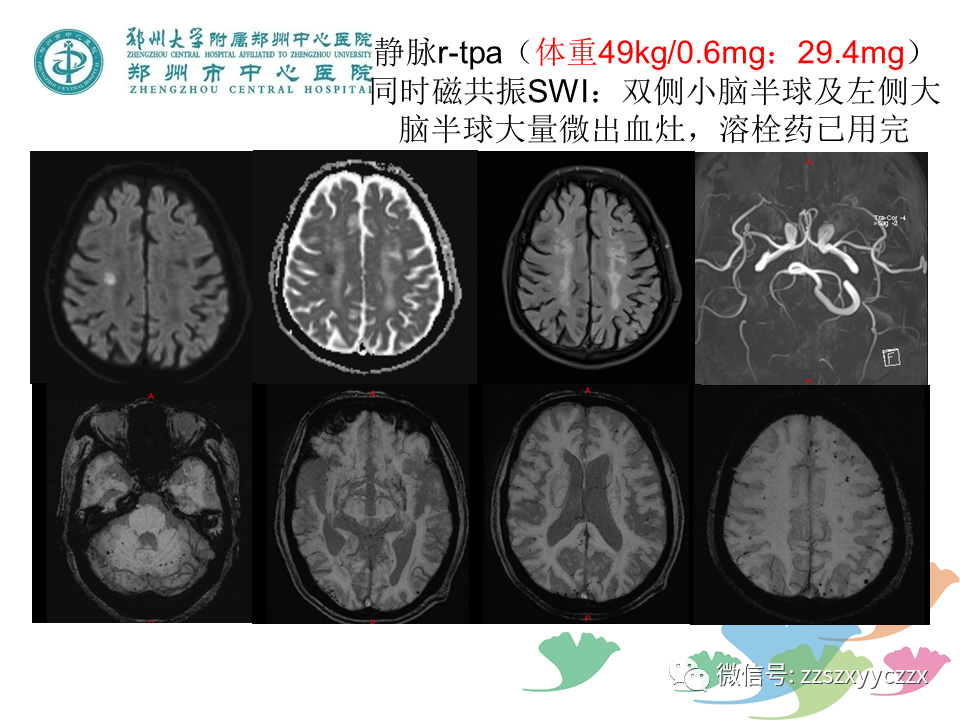
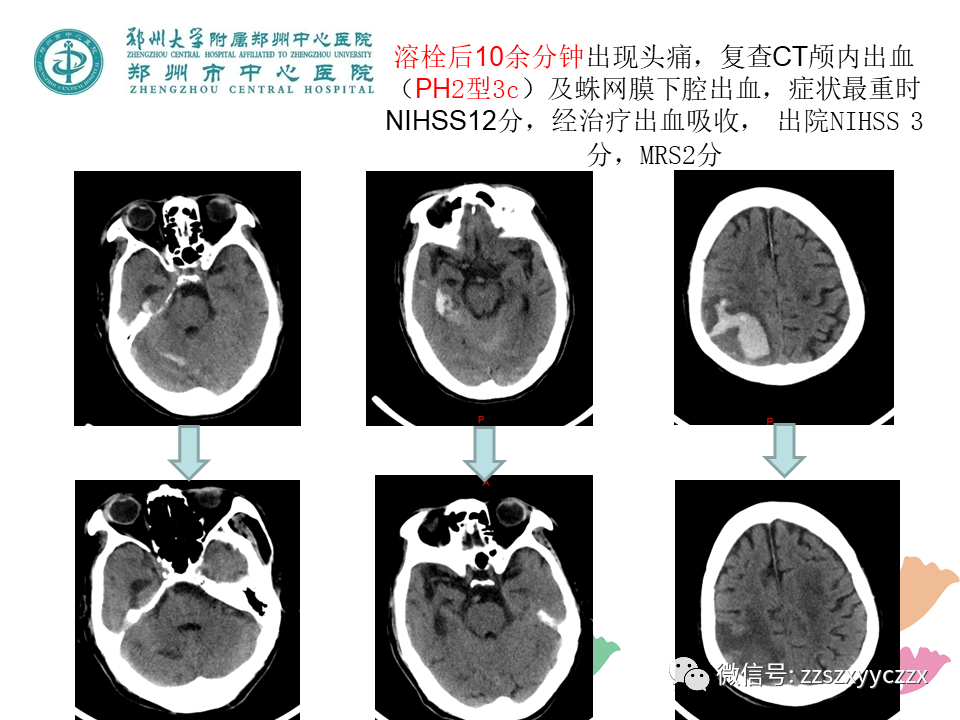
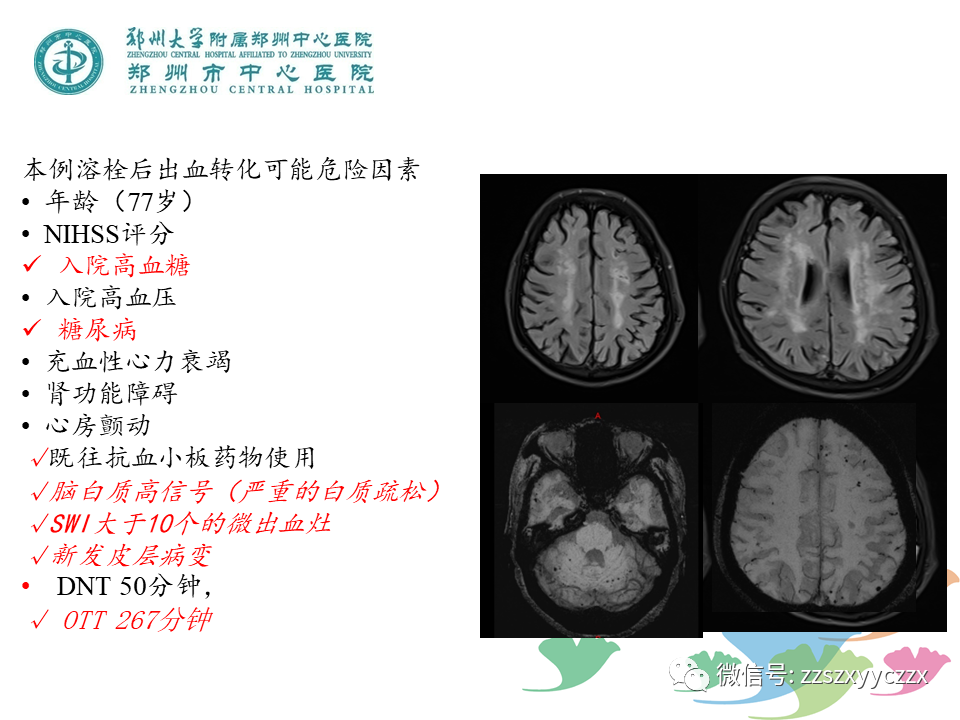
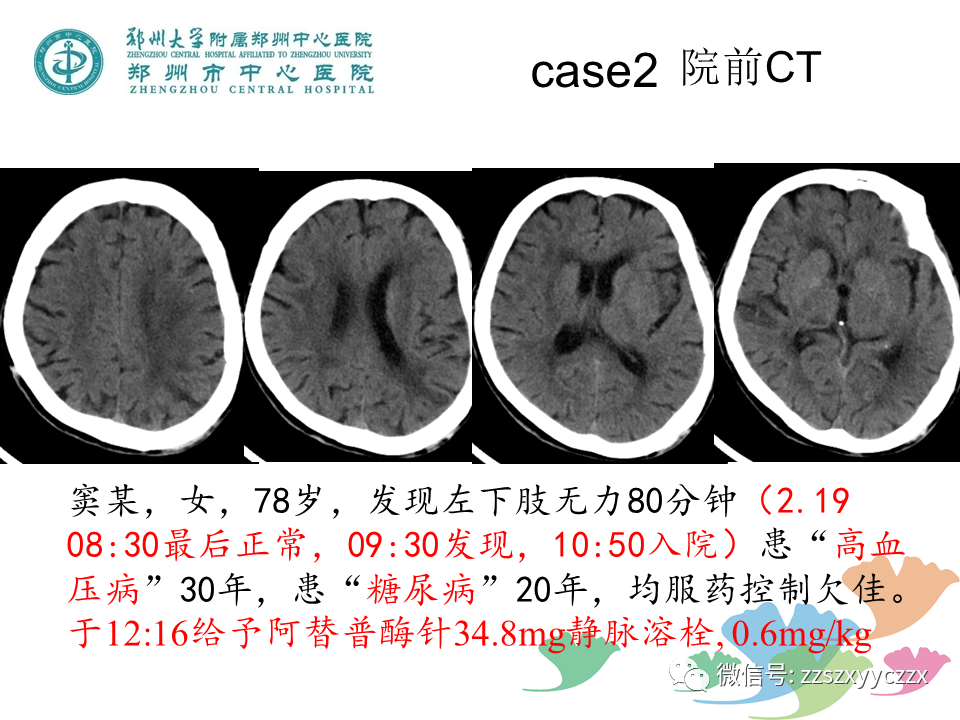
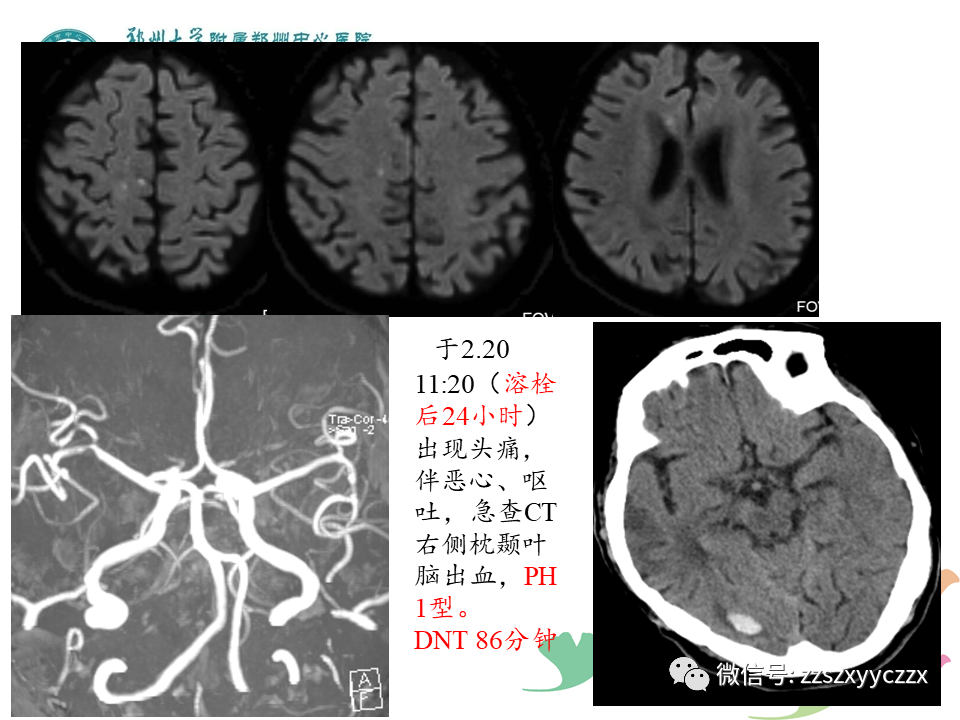
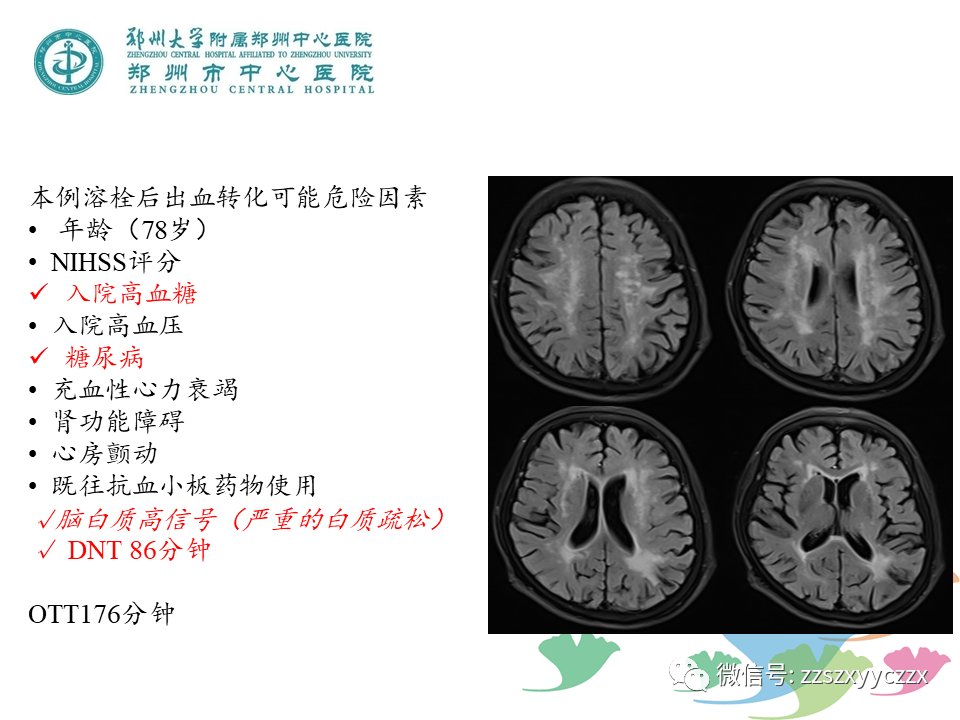
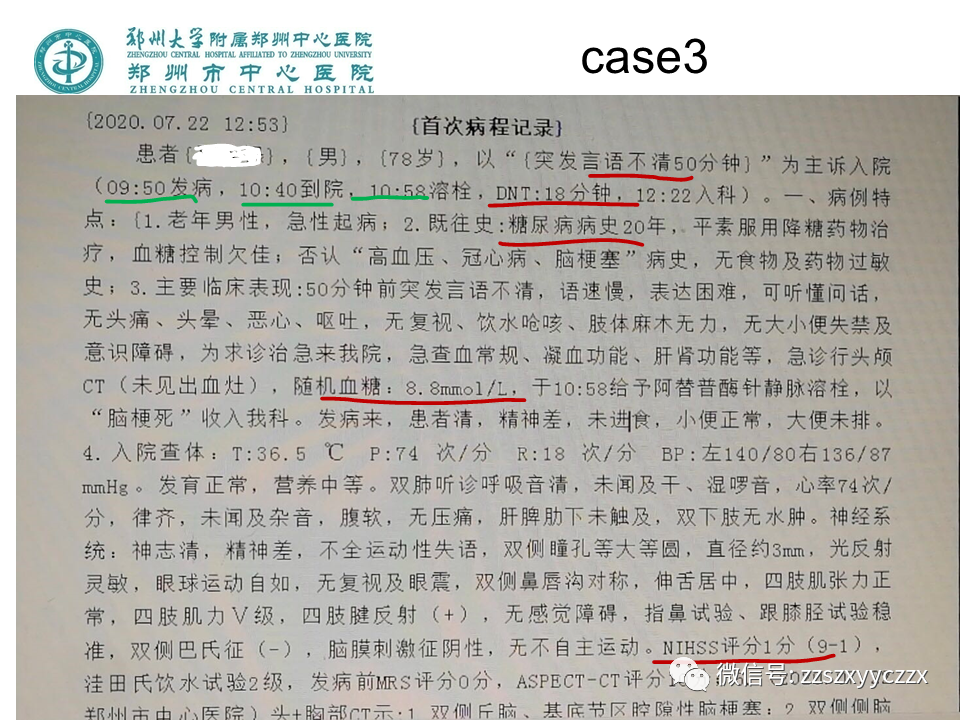
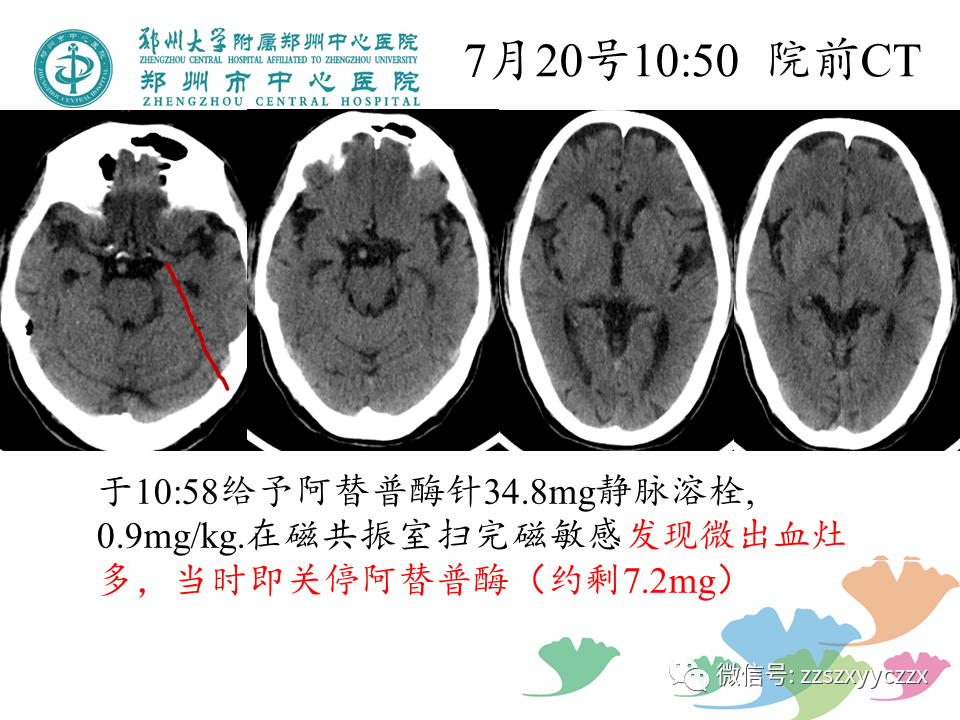
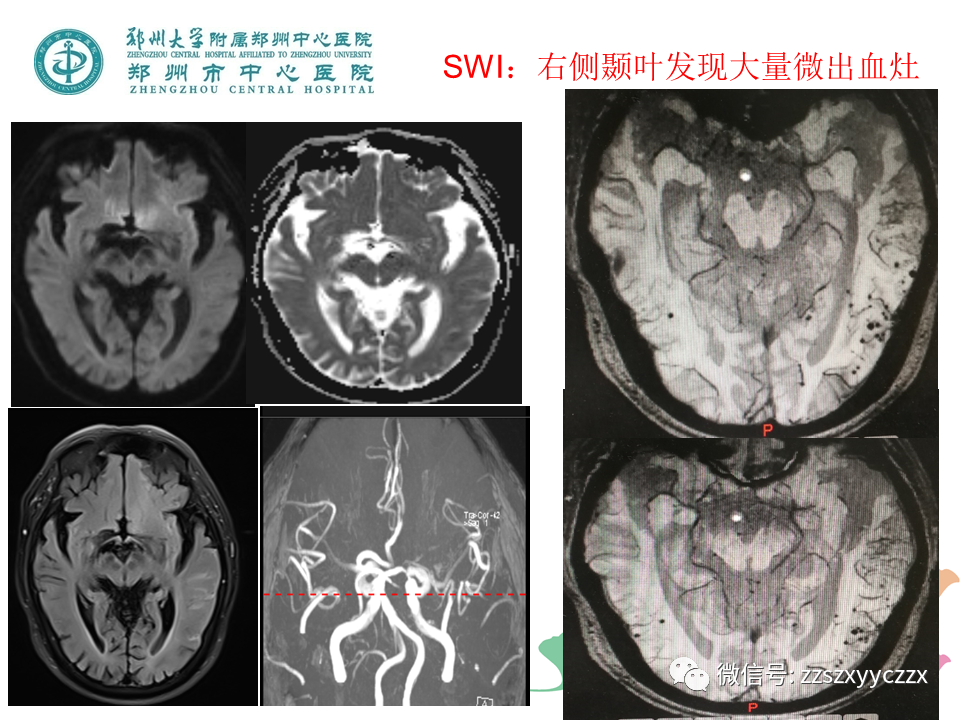
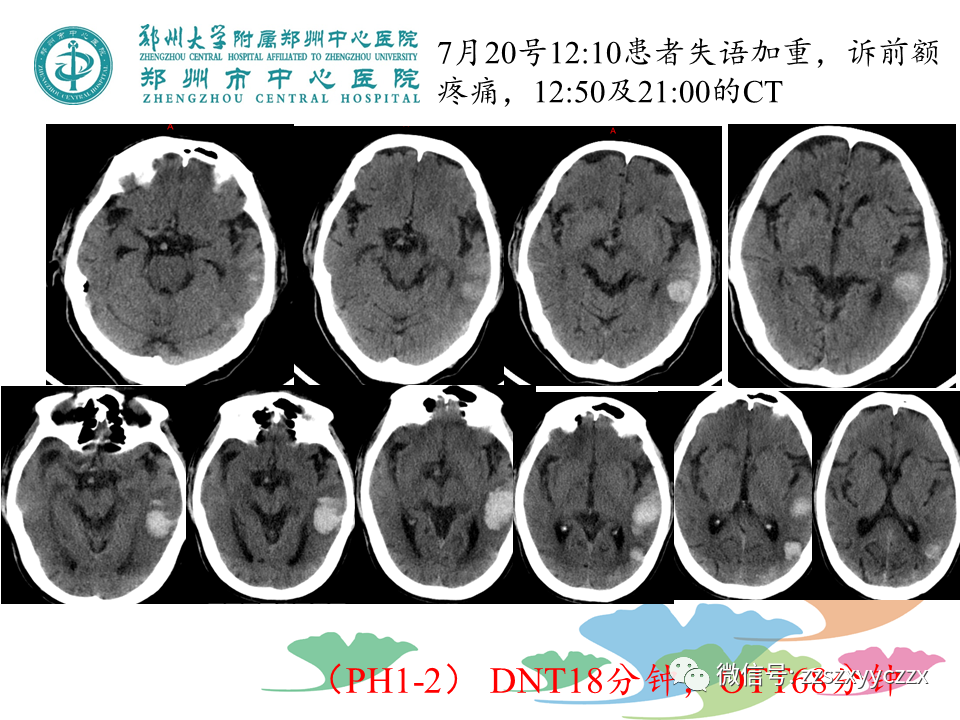
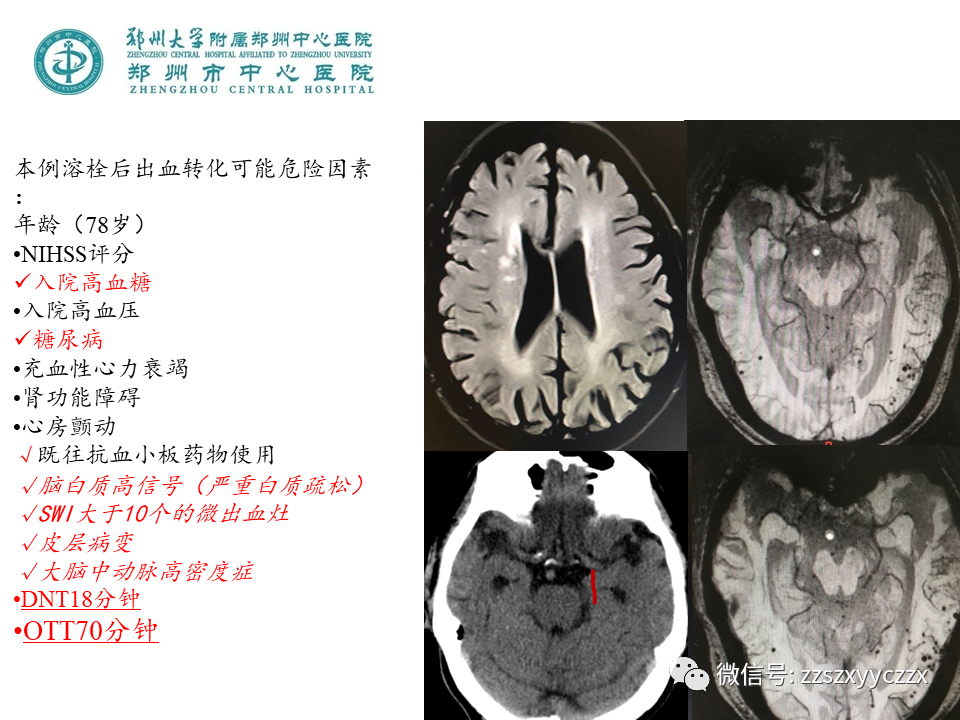
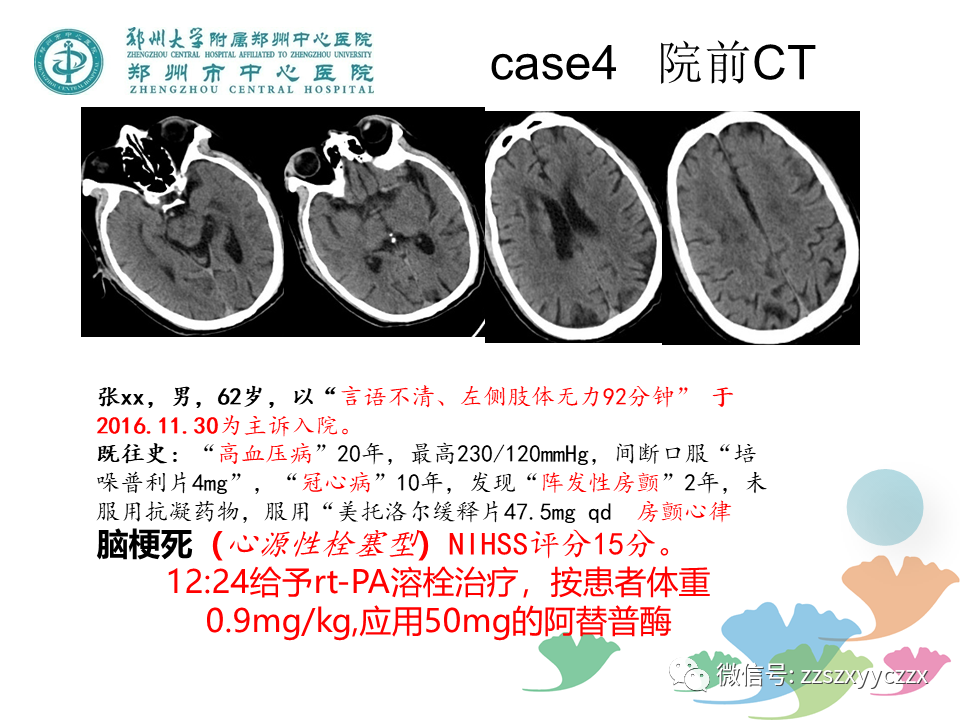
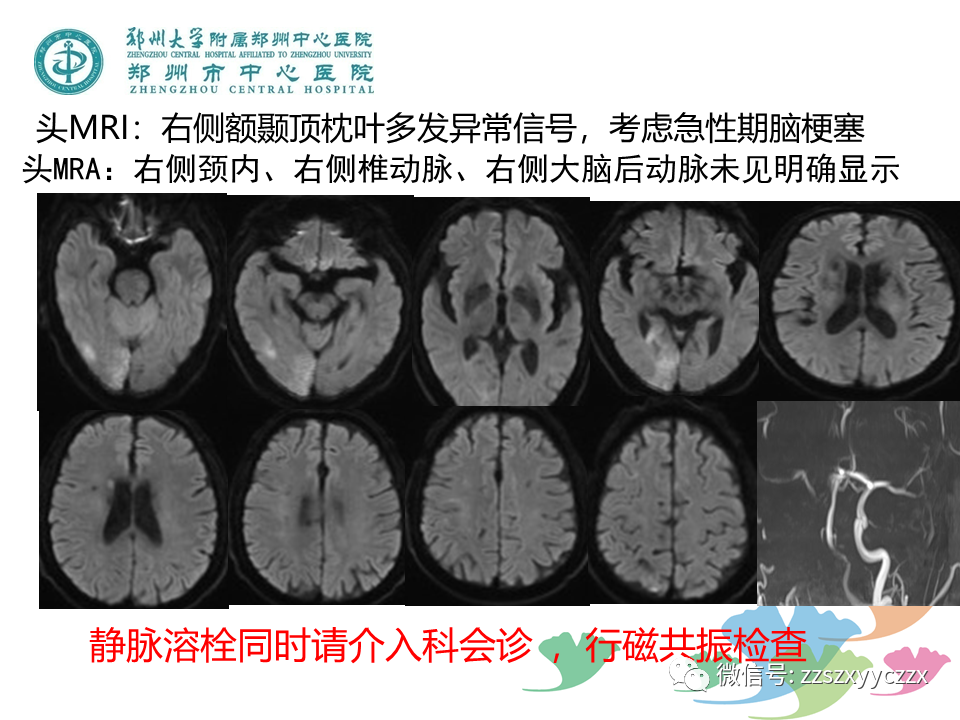
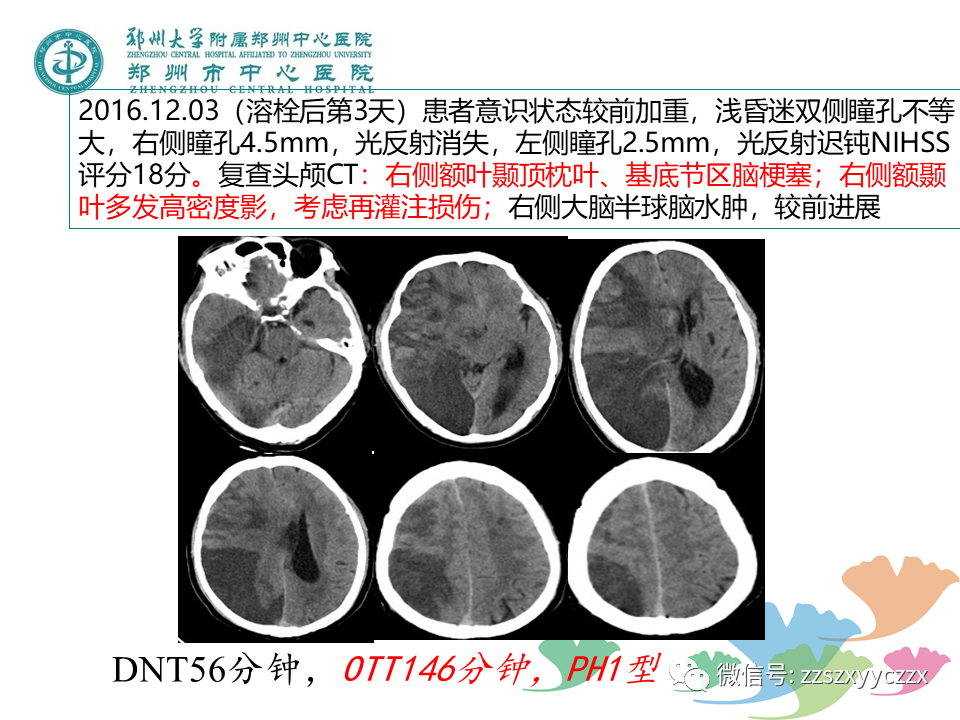
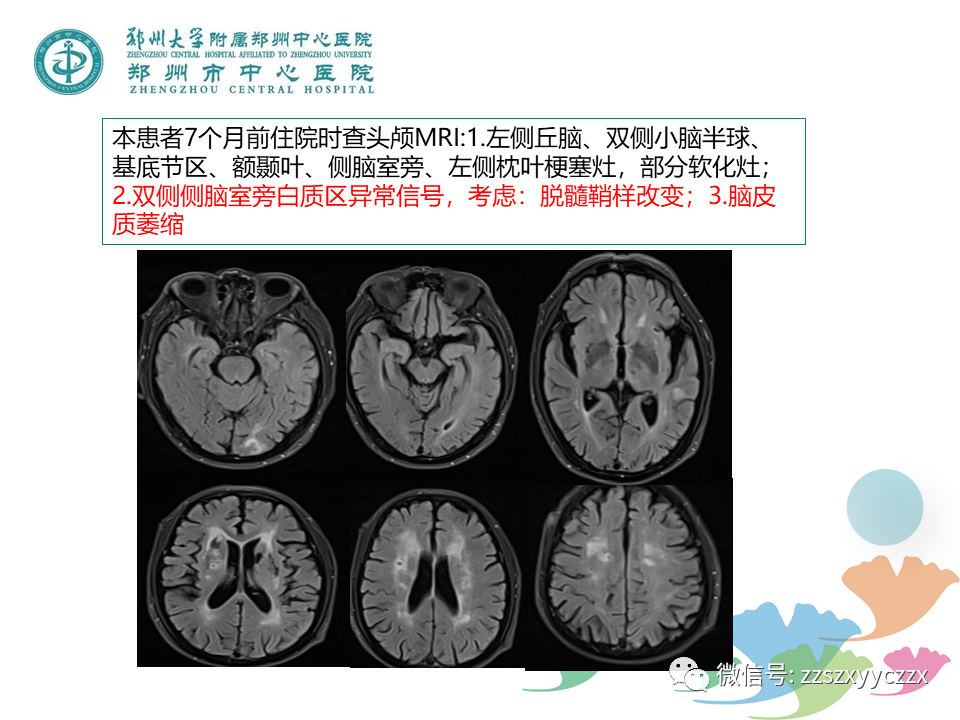
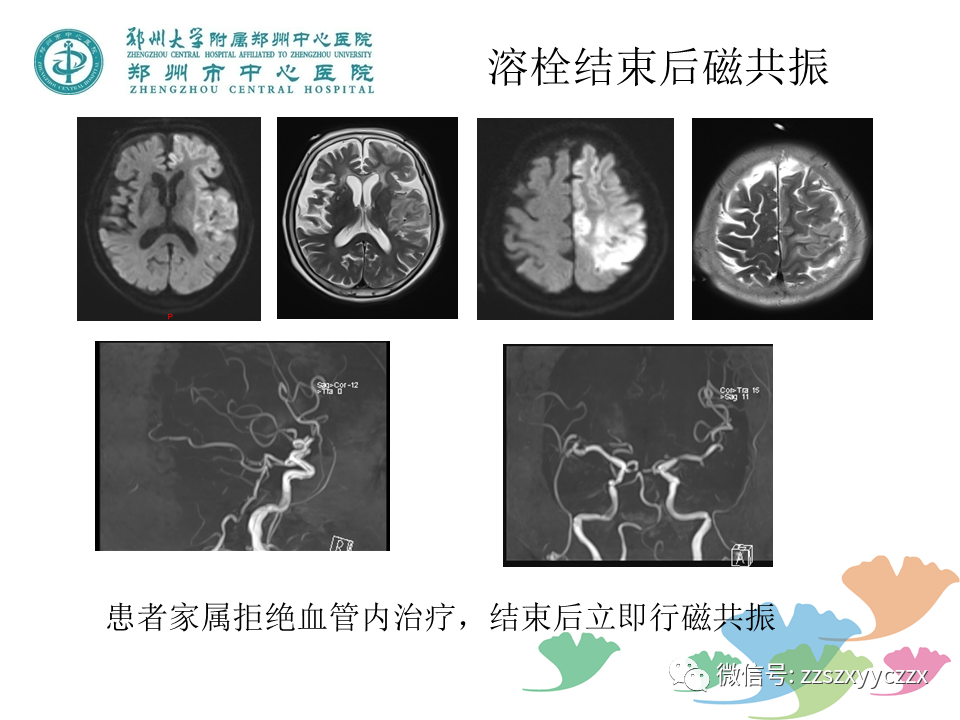
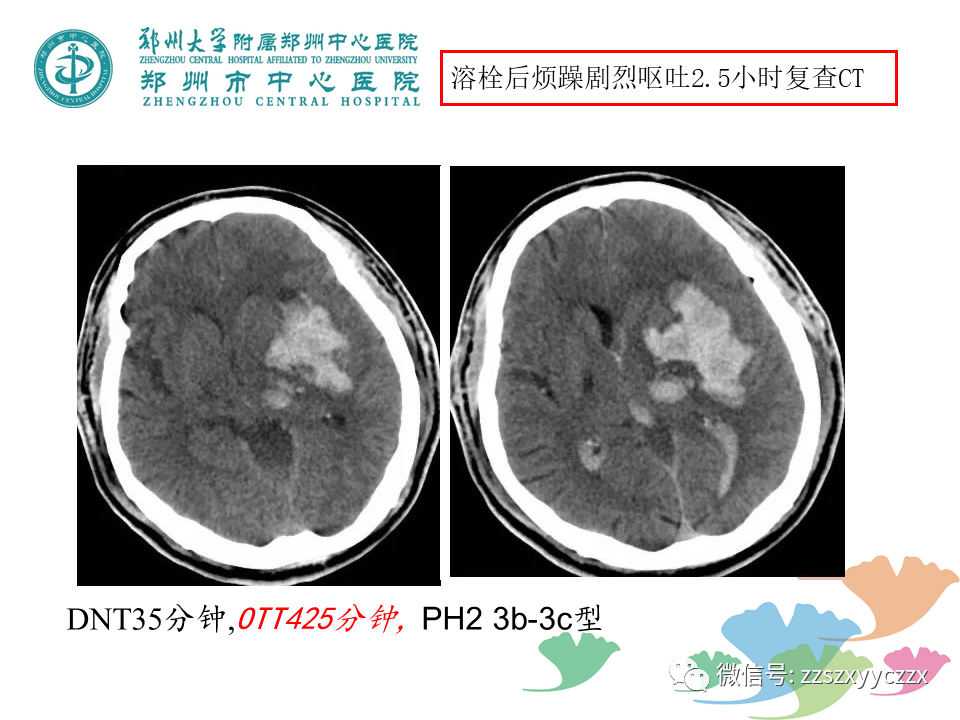
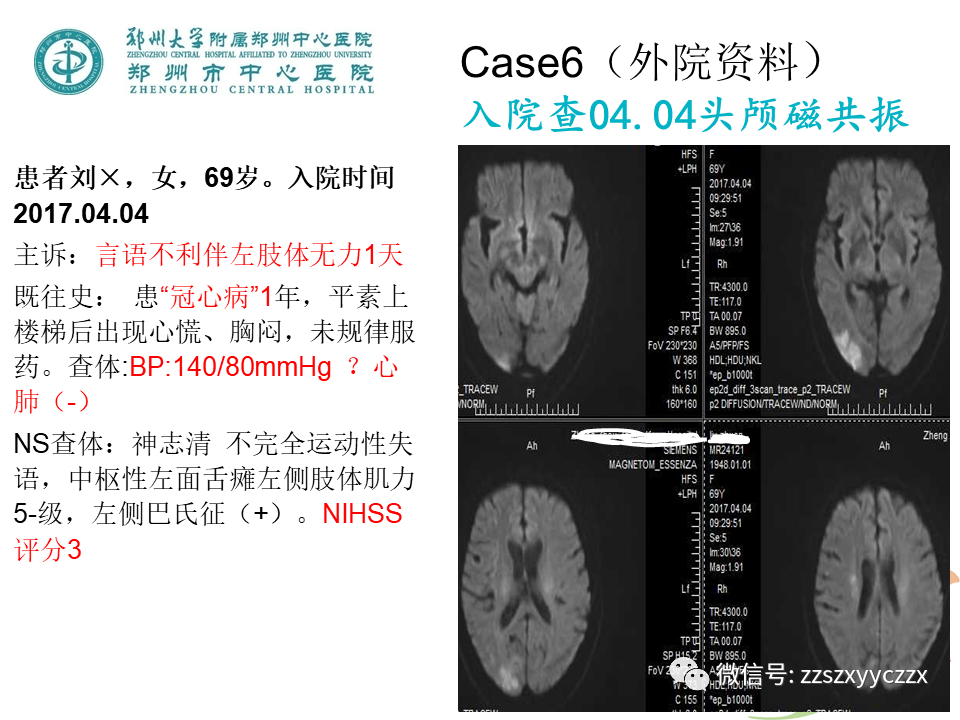
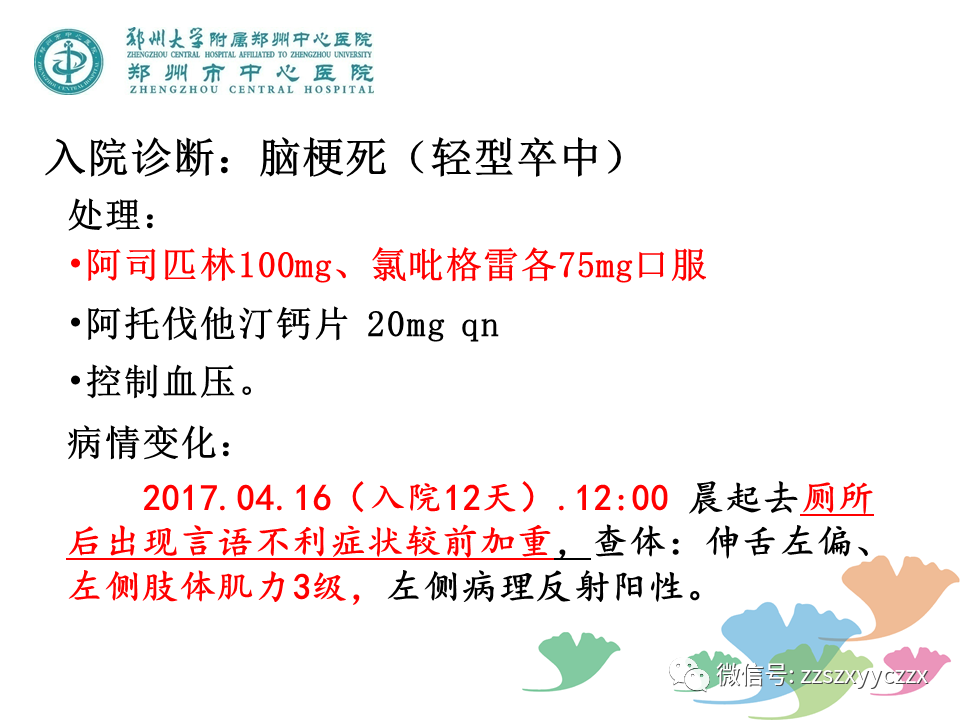
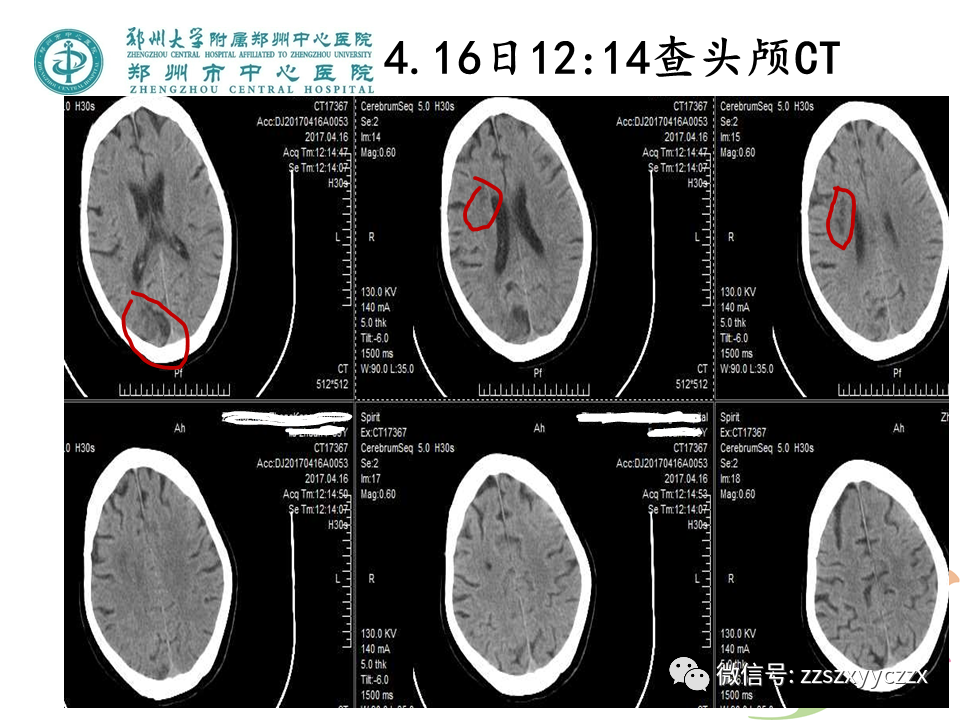
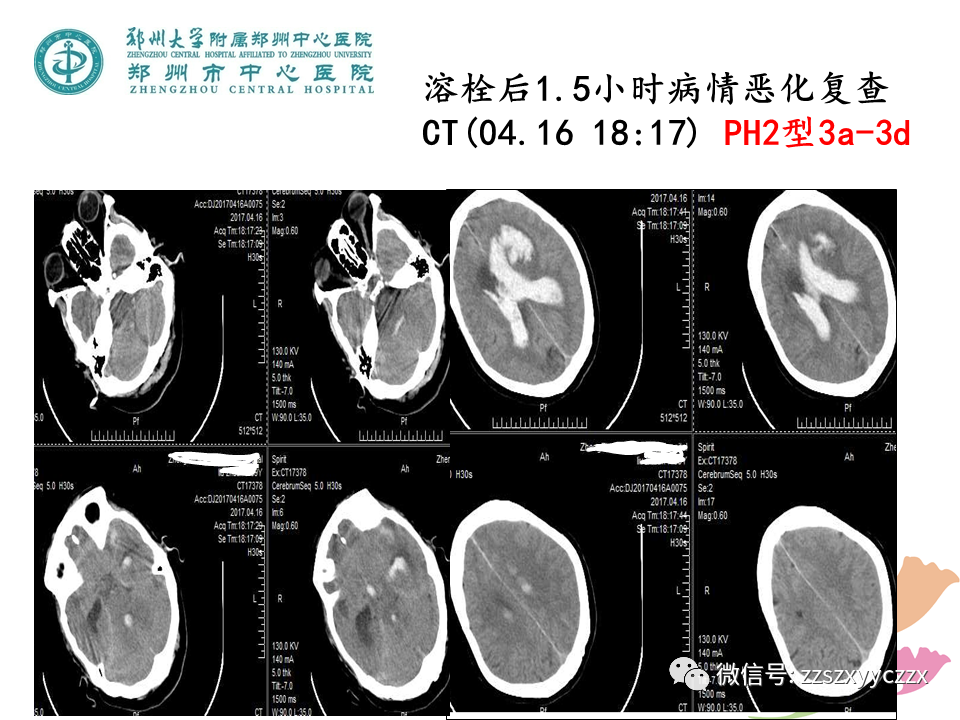
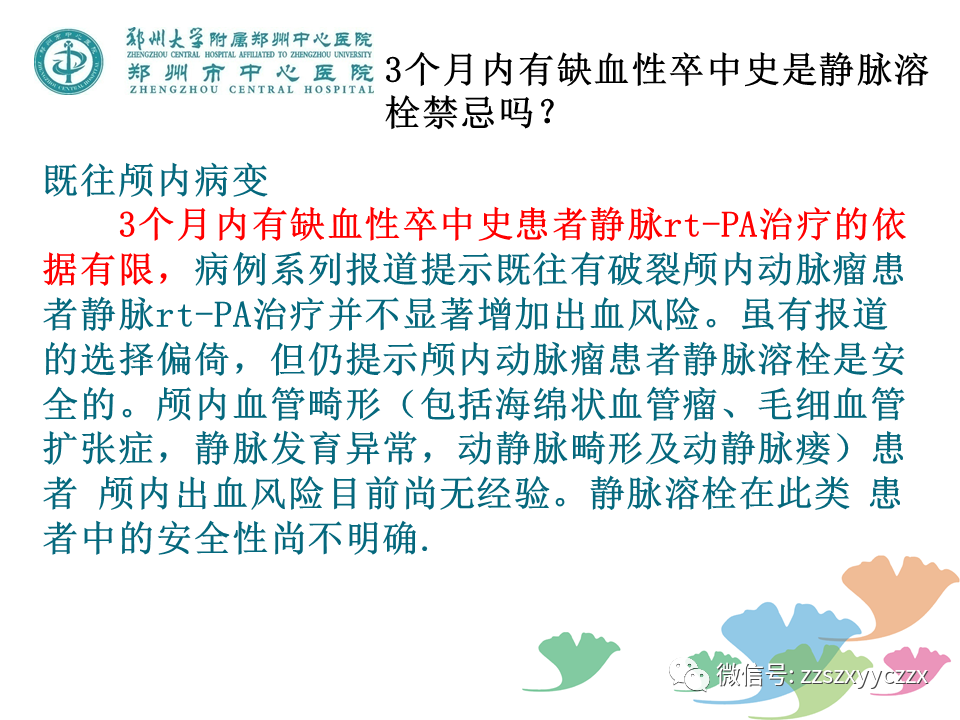
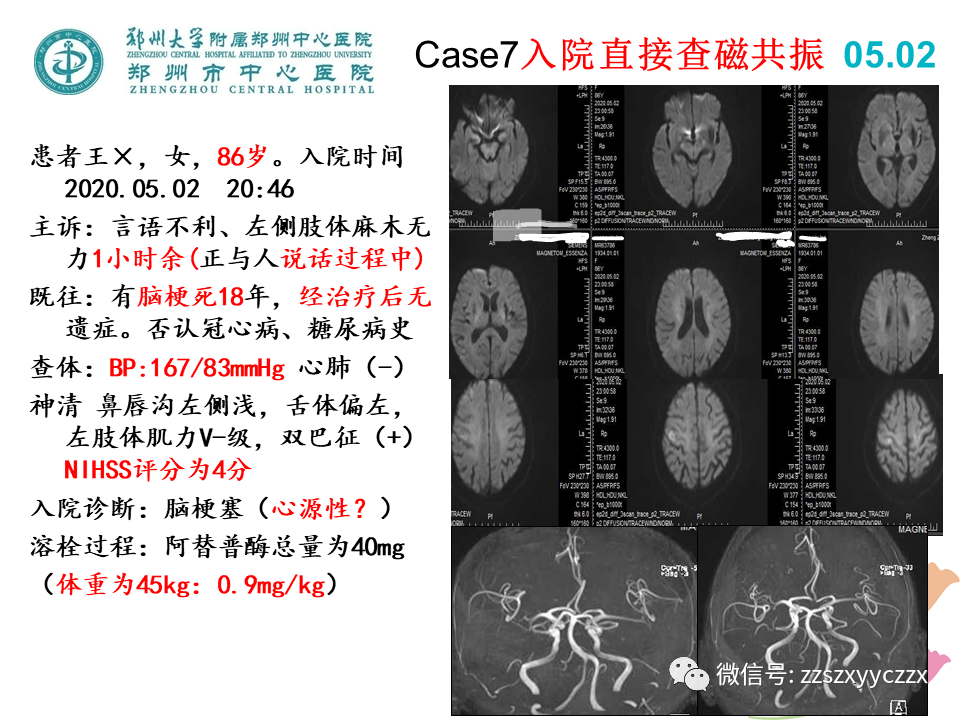
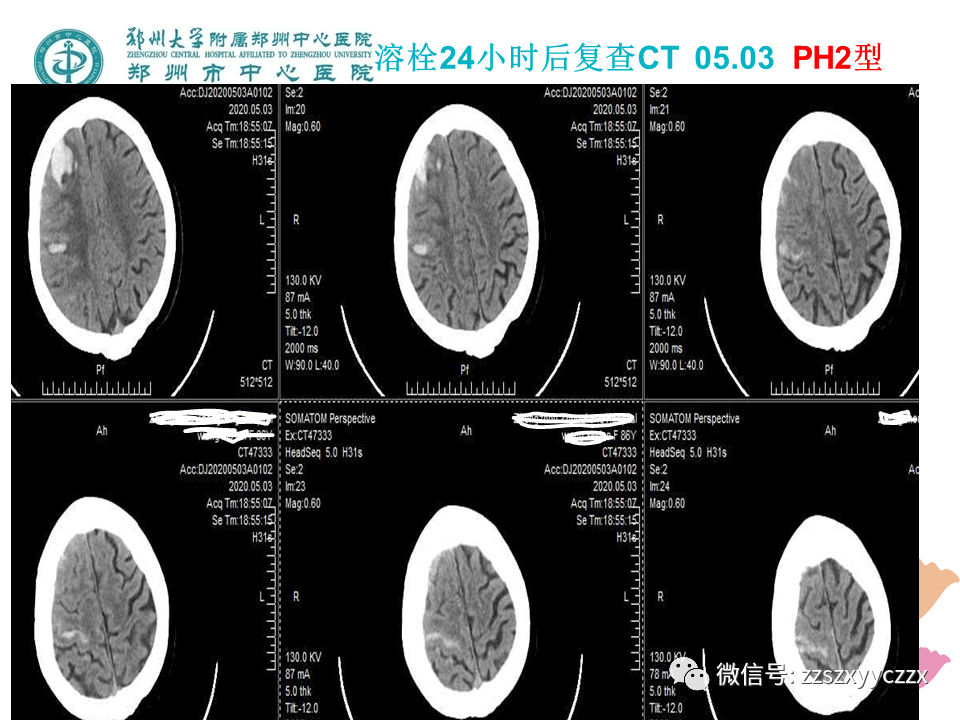
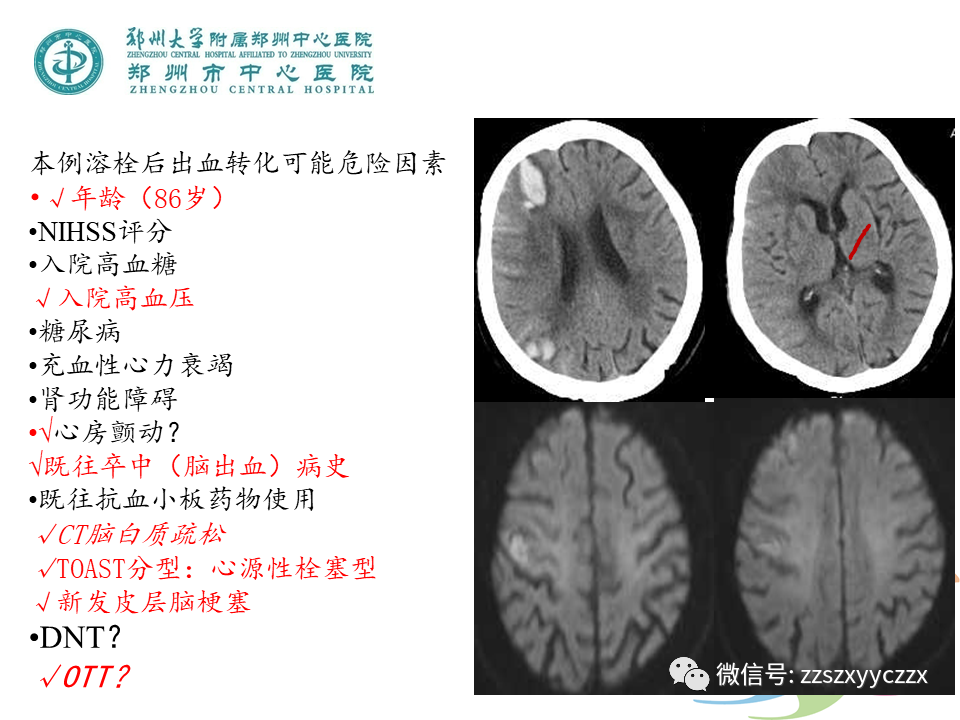
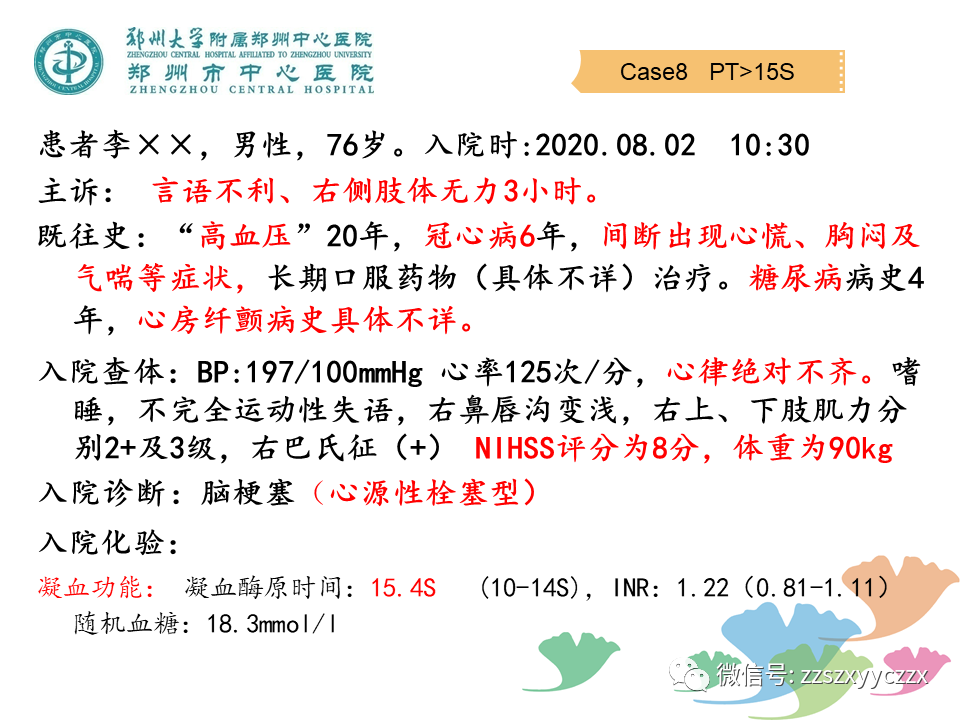
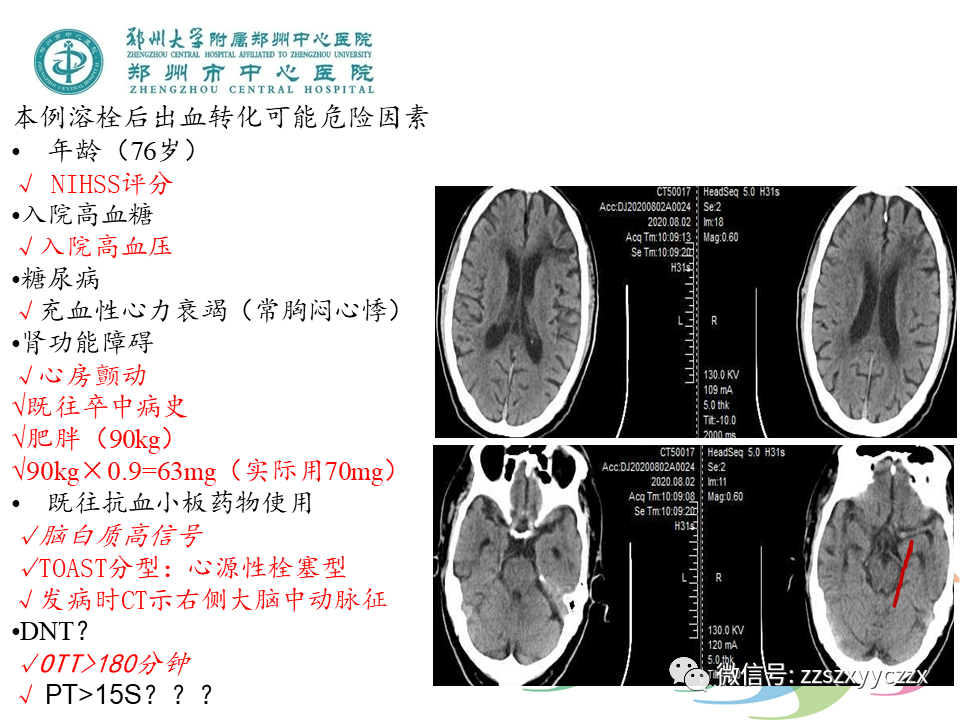
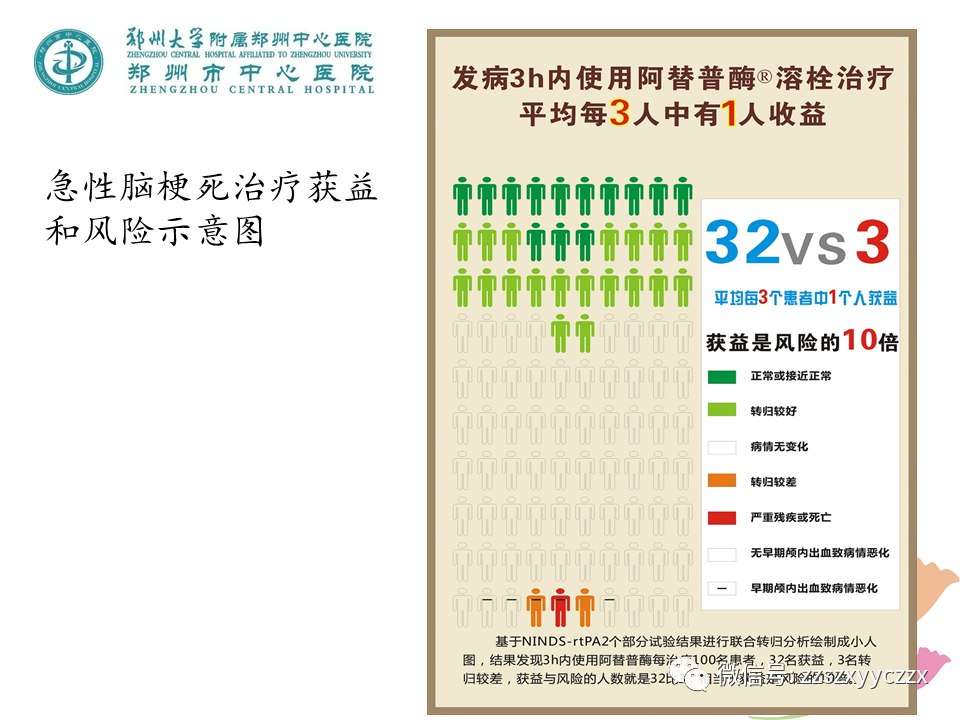
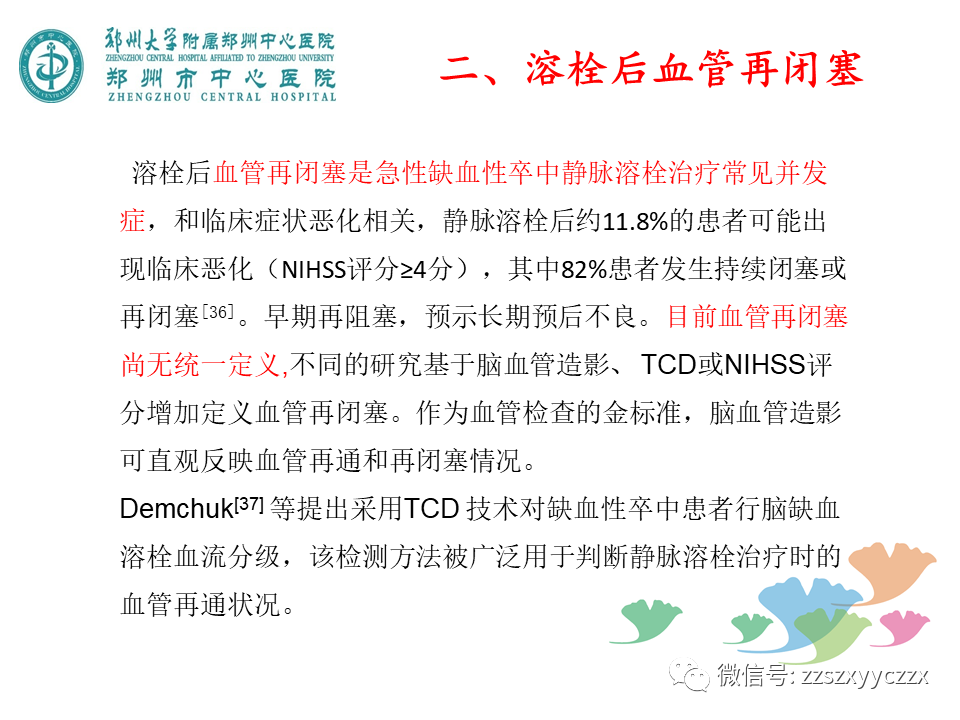
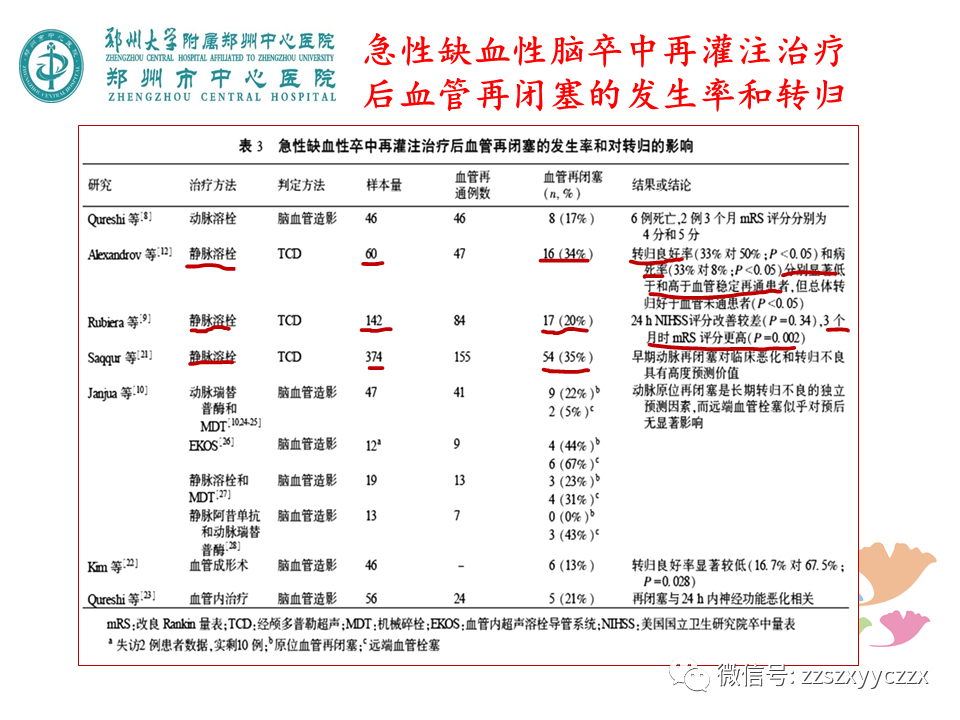
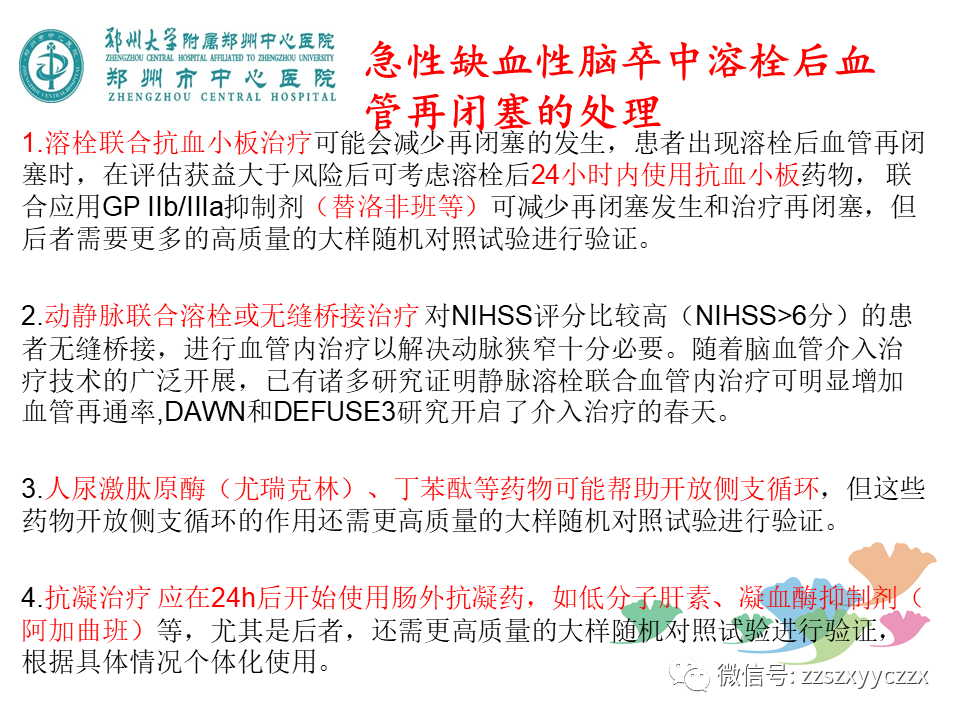
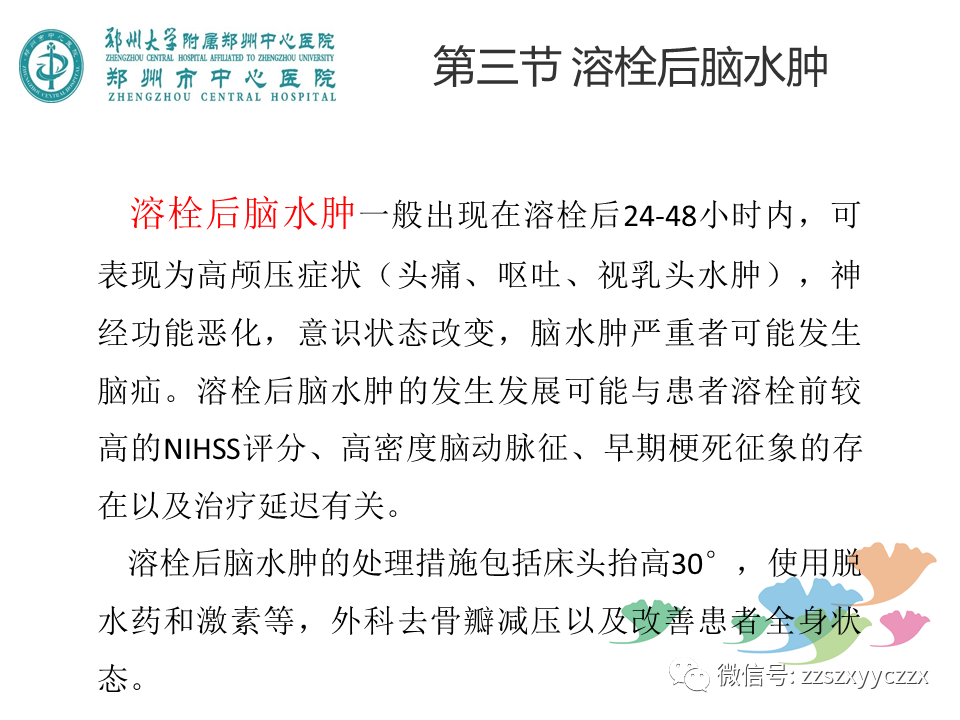
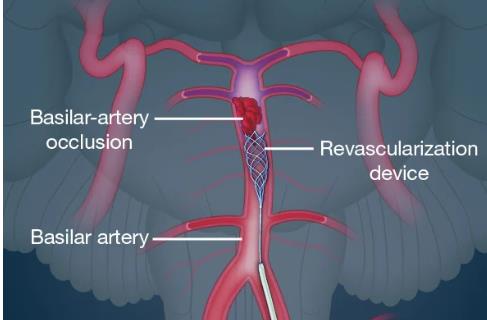
静脉溶栓治疗急性缺血性脑卒中,是目前最有效的治疗办法,但静脉溶栓带来的并发症不容忽视,其中脑出血转化、血管再闭塞、溶栓后脑水肿等是静脉溶栓后常见的并发症
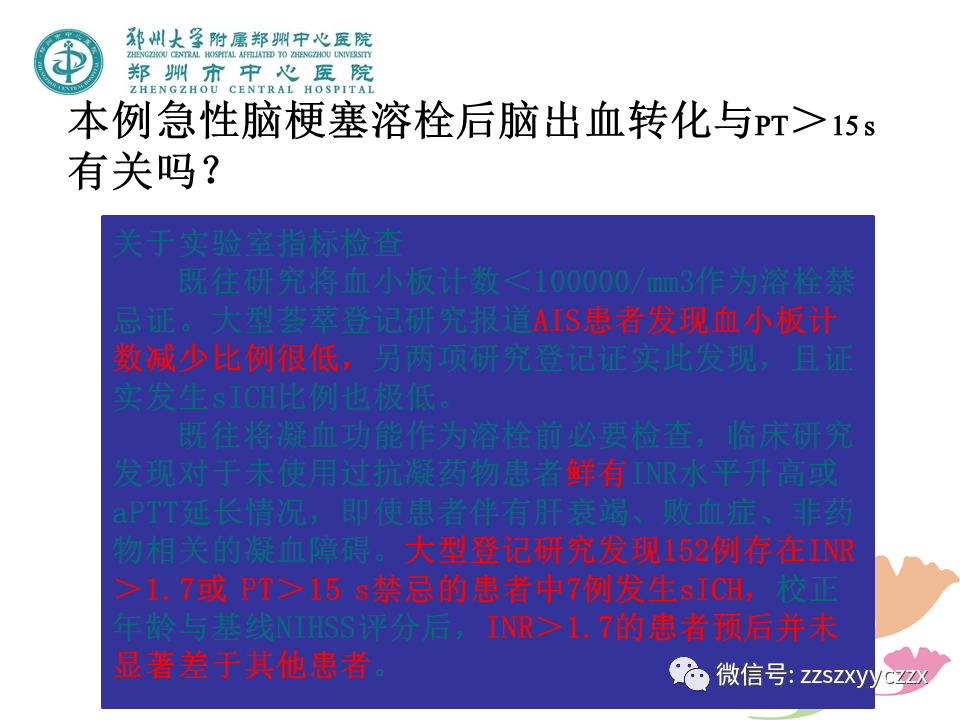
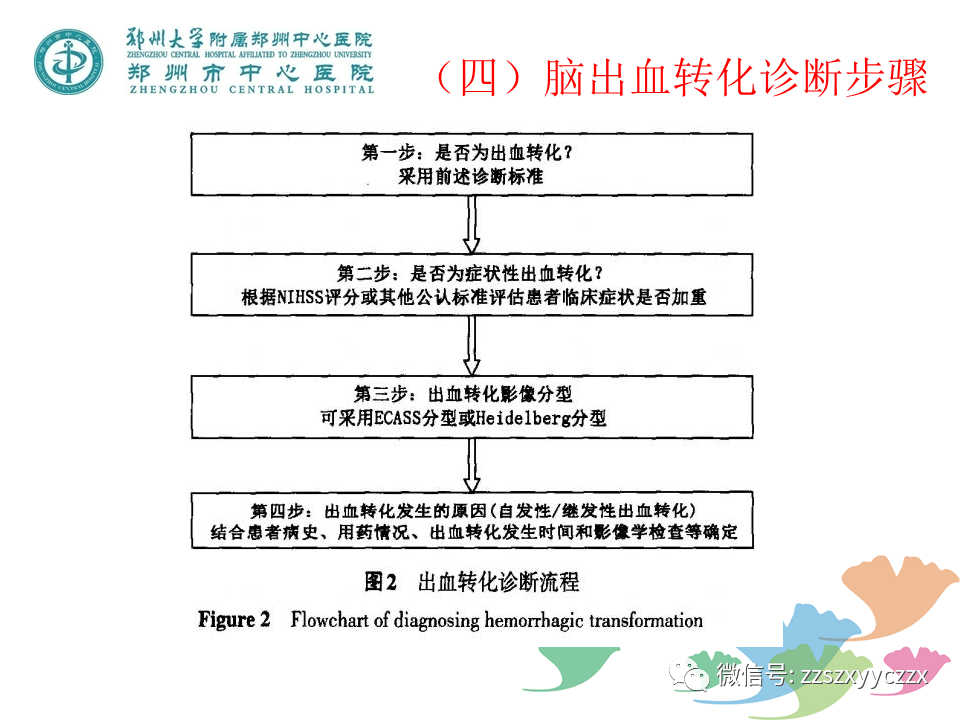
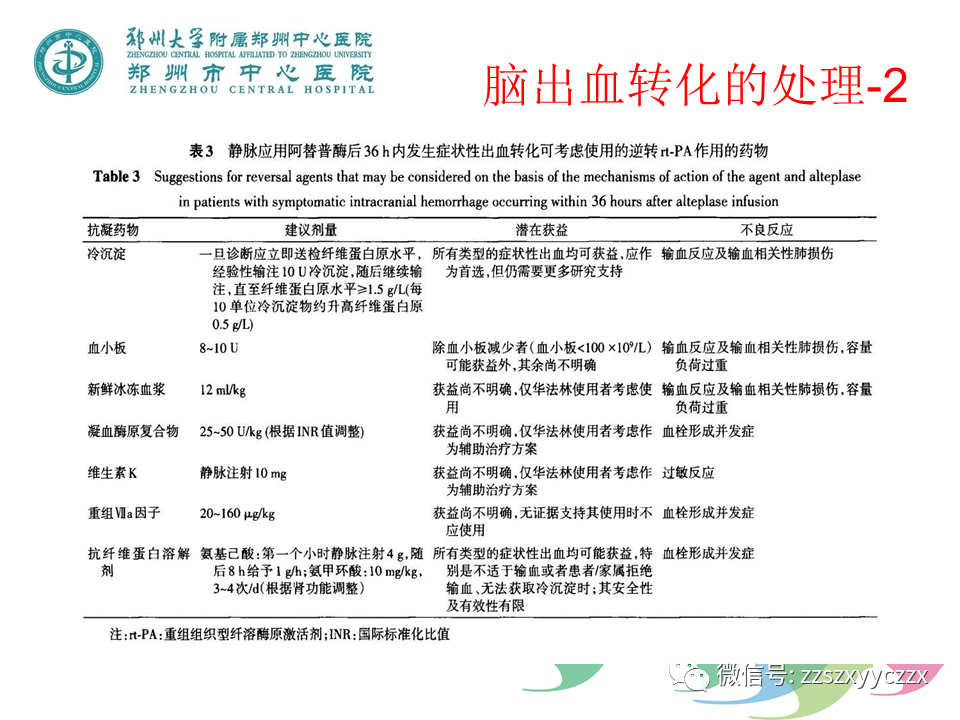
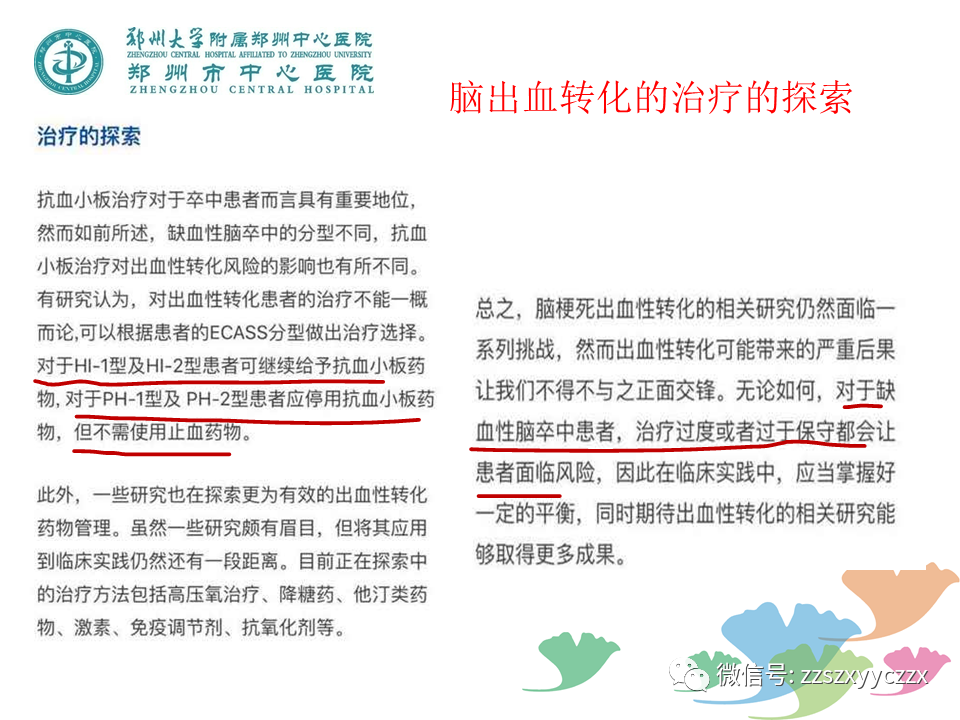
静脉溶栓治疗急性缺血性脑卒中,是目前最有效的治疗办法,但静脉溶栓带来的并发症不容忽视,其中脑出血转化、血管再闭塞、溶栓后脑水肿等是静脉溶栓后常见的并发症,本文对这些并发症进行预警和处理,为临床提供参考。

















本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#并发#
35
#PPT#
52
#静脉#
44
学习
61
默里大学下属的非营利组织DRIVE(Drug
62
厉害了,又学习了
64