Blood:Daratumumab,为T-ALL患者带来新的治疗希望。
2018-01-07 MedSci MedSci原创
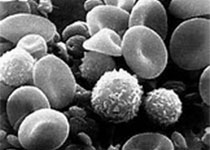
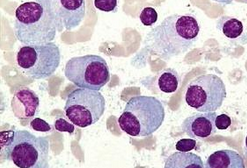
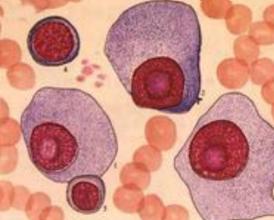
由于获得性或本身携带的疾病耐药性,使得复发性/难治性T细胞急性淋巴细胞白血病(T-ALL)患者的预后极差。故急需研发新型低毒性的药物。目前,癌症治疗最有希望的一种新兴治疗策略——靶向免疫疗法。免疫疗法可提高其他恶性血液肿瘤(包括B-ALL)患者的预后,但,目前尚无免疫疗法可改善T-ALL的预后。Karen L. Bride等人猜想靶向CD38或许可有效对抗T-ALL。其已通过实验证实,来源于T-A
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#mAb#
47
学习了谢谢作者分享!
51
#ALL#
27
#Daratumumab#
33
#T-ALL#
45
不错的文章值得推荐
57
由于获得性或本身携带的疾病耐药性.使得复发性/难治性T细胞急性淋巴细胞白血病(T-ALL)患者的预后极差
60