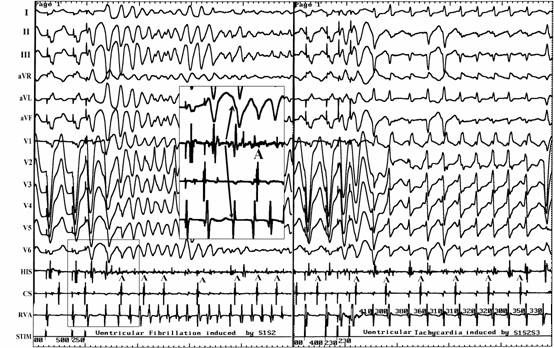
Circulation:窦性心律传导异常点指导的室速的靶向消融
2019-10-24 梅梅 梅斯原创
准确和快速的识别最容易再起搏的瘢痕区域是指导室性心动过速(,简称室速,VT)射频消融的必要条件。研究人员前瞻性评估了窦性心律时,靶向心室激动传导分析所鉴定的减速带(DZ)进行的VT射频消融的预后。本研究招募了120位瘢痕相关的室速患者(中位年龄65岁[59-71],15%的女性,50%的非缺血性,中位射血分数为31%),共进行了144次射频消融。57%的患者既往进行过射频消融,59%的患者有心外膜
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#消融#
24
#窦性心律#
38
#室速#
50
好
69