睡眠浅,越睡越累?哈佛医学院首次定位大脑深度睡眠关键蛋白,提供失眠新疗法
2022-05-04 乐一 MedSci原创
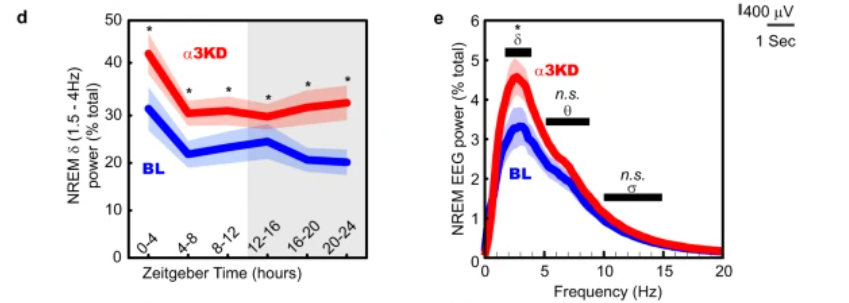
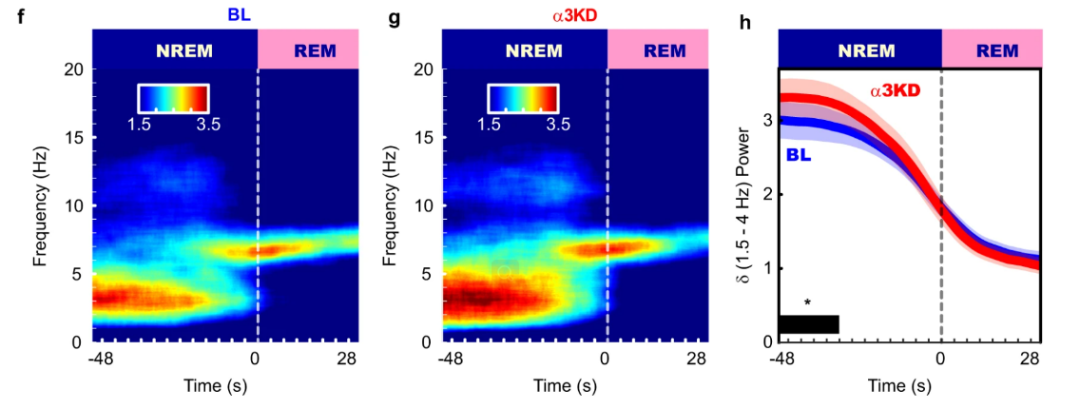
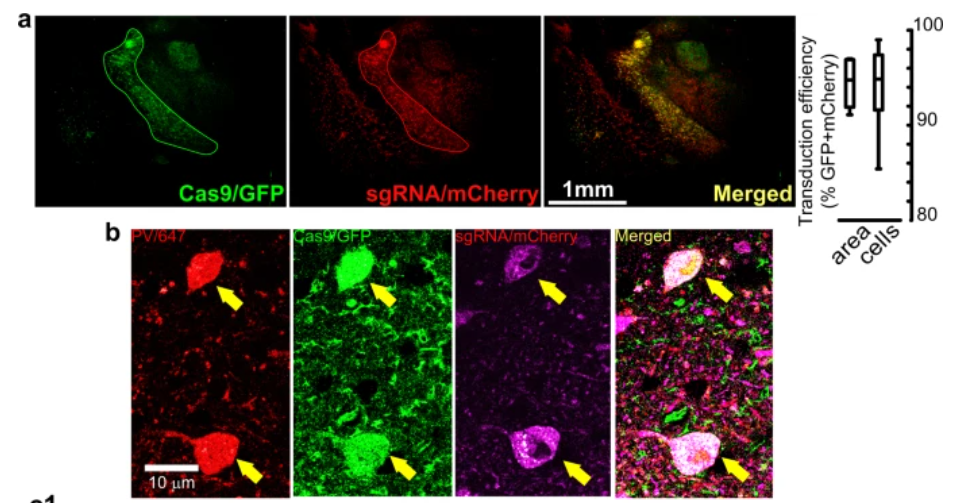
Nature Communications:通过对丘脑网状神经元上的GABAA alpha3亚基进行敲除,可有效增强小鼠的深度睡眠。

(图片来源:Nature Communications)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#关键蛋白#
35
#医学院#
37
#哈佛医学院#
33
#新疗法#
48
#哈佛#
27
mark学习
46