炎症负荷指数:肿瘤,以及多种慢性疾病预后预测因子
2024-02-10 MedSci原创 MedSci原创 发表于威斯康星
首都医科大学附属北京世纪坛医院石汉平教授团队开发了一种评估肿瘤患者炎症负荷的工具——炎症负荷指数(inflammatory burden index,IBI),即C反应蛋白、中
首都医科大学附属北京世纪坛医院石汉平教授团队开发了一种评估肿瘤患者炎症负荷的工具——炎症负荷指数(inflammatory burden index,IBI),即C反应蛋白、中性粒细胞和淋巴细胞的组合,并证实其是肿瘤患者强有力的预后预测指标。与目前现有的系统性炎症生物标志物相比,IBI是预测肿瘤预后最佳的生物标志物。
在线使用:炎症负荷指数(inflammatory burden index,IBI)
2022年10月,石汉平教授团队的一项最新成果发表在临床营养领域国际权威期刊《Clinical Nutrition》上,研究还首次建立了一种新的炎症负荷指数(Inflammatory burden index,IBI),据此将恶性肿瘤分为高、中、低炎症负荷三种类型,为创新肿瘤治疗提供了重要思路。
石汉平教授团队开发了一种评估肿瘤患者炎症负荷的工具IBI。即C反应蛋白、中性粒细胞和淋巴细胞的组合[计算公式为IBI=C反应蛋白(C-reactive protein,CRP)×中性粒细胞/淋巴细胞],并证实其是肿瘤患者强有力的预后预测指标。与目前现有的系统性炎症生物标志物相比,IBI是预测肿瘤预后最佳的生物标志物。根据IBI可以对不同恶性肿瘤进行炎症负荷分级,并实现了良好的预后分层。
研究者评估了IBI评分与生活功能、营养状况、短期结果、住院时间和住院费用等的关系,为综合评估IBI在恶性肿瘤中的预后价值和临床应用提供了有价值的参考。 在精准医学时代,这些分析对于肿瘤患者的疗效监测、预后指导和治疗干预具有重要的临床价值和意义。在临床上,我们可以用IBI来监测患者接受手术、化疗或放疗等抗癌治疗后的治疗效果,对于那些治疗后持续IBI升高的患者,可能需要考虑更强的治疗方案。另外在患者入院时,IBI还可以作为评估患者炎症负荷水平的工具,对于那些IBI高的患者,可以考虑降炎治疗。
在结直肠癌的预后判断上,IBI>33.68(HR=3.576,95%CI:3.114~4.138)是影响结直肠癌患者预后的独立危险因素。
使用R软件包rms,整合生存时间、生存状态以及T分期、N分期和IBI 3个特征的数据,基于Cox回归建立了列线图模型(图2A),模型总体的C-index为0.849(95%CI:0.829~0.868,P<0.001);同时绘制了12、36和60个月的校准曲线,显示预测生存率与实际生存率之间具有良好的一致性,见图2B。同时绘制12、36和60个月的生存ROC曲线,3者的AUC分别为0.77(95%CI:0.71~0.88)、0.81(95%CI:0.77~0.89)和0.85(95%CI:0.78~0.92),均具有良好的预测价值,见图2C。
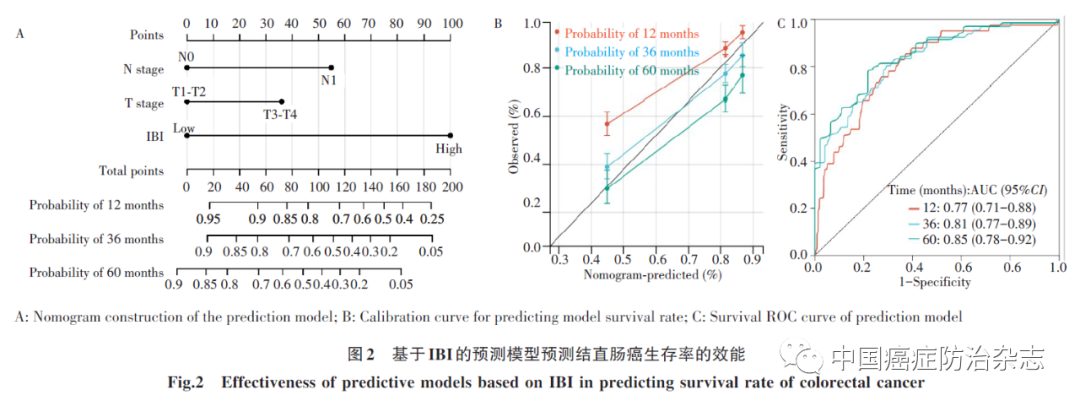
IBI>33.68是结直肠癌患者预后的独立危险因素,而且IBI具有良好的诊断及预后预测价值,可能是结直肠癌一种新型的有效生物标志物。
与目前现有的系统性炎症生物标志物相比,IBI是预测肿瘤预后最佳的生物标志物。研究者根据IBI对不同恶性肿瘤进行炎症负荷分级,并实现了良好的预后分层 (如图)。此外,研究者评估了IBI评分与生活功能、营养状况、短期结果、住院时间和住院费用等的关系,为综合评估IBI在恶性肿瘤中的预后价值和临床应用提供了有价值的参考。最后,研究者使用内部随机验证队列证实了新开发的IBI在恶性肿瘤预后评估中具有良好临床应用前景。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















学习谢谢分享。
12
北京世纪坛医院石汉平教授团队
21
\兴学学习
18
学习
23
#肿瘤# #炎症# #炎症负荷指数#
38