索拉非尼可改善纤维瘤患者的无进展生存期
2018-04-03 MedSci MedSci原创
近日,一项随机临床试验显示,与安慰剂组相比,索拉非尼甲苯磺酸盐可显著延长硬纤维瘤或侵袭性纤维瘤(DT/DF)患者的无进展生存期,无进展生存期是患者在疾病恶化之前存活的时间长度。
索拉非尼可改善纤维瘤患者的无进展生存期
近日,一项随机临床试验显示,与安慰剂组相比,索拉非尼甲苯磺酸盐可显著延长硬纤维瘤或侵袭性纤维瘤(DT/DF)患者的无进展生存期,无进展生存期是患者在疾病恶化之前存活的时间长度。
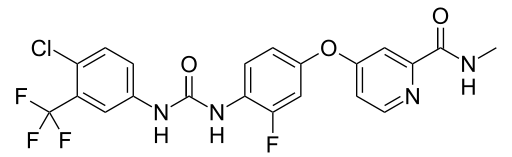
索拉非尼是一种口服给药的靶向治疗药物,能够干扰肿瘤生长需要的新生血管的生长。它被美国食品和药物管理局批准用于治疗晚期肾癌、肝癌和甲状腺癌的患者。之所以选择索拉非尼进行该项临床试验,是因为在之前对索拉非尼治疗的患者进行的回顾性研究中,研究人员发现患者的硬纤维瘤缩小,患者疼痛和其他症状减轻。
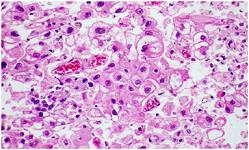
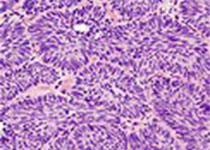
纽约纪念斯隆凯特琳癌症中心的肿瘤医学家,首席研究员Mrinal M. Gounder博士说:“这个III期临床试验的良好结果代表了硬纤维瘤患者治疗方法的正式转变,索拉非尼是一种治疗这种罕见癌症的新方式”。在美国,每年约有1000例患者被确诊为DT/DF,其中许多患者相对年轻。纤维瘤通常出现在四肢或腹部,偶尔与家族性腺瘤性息肉病或Gardner综合征相关。DT/DF具有局部侵袭性,可导致疼痛并降低移动性,并可侵入重要组织或器官,导致肠梗阻和其他严重并发症。
原始出处:
https://www.europeanpharmaceuticalreview.com/news/74135/sorafenib-improves-rare-sarcomas/
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#生存期#
26
#纤维瘤#
31
#无进展生存期#
34
学习
62
不错耶.学习了
48