中国学者:ARB降压药或可降低房颤合并高血压患者死亡率
2022-09-15 MedSci原创 MedSci原创 发表于上海
除了血压控制治疗外,预防 RAAS 系统的激活可能会改善房颤和高血压患者的预后。这些结果为房颤合并高血压患者的三级预防治疗提供了证据。
肾素-血管紧张素-醛固酮系统(RAAS)为体内的一种调控血管内容量、钠钾离子平衡的调节体系,引起血管平滑肌收缩及水、钠重吸收,产生维持血容量及动脉血压的作用。RAAS抑制剂对房颤一级和二级预防的作用已得到充分的研究。然而,血管紧张素转化酶抑制剂(ACEI)和血管紧张素受体拮抗剂(ARB) 对房颤患者死亡率的影响仍不清楚。
近期,发表在BMC Cardiovasc Disord 杂志的一项研究,探讨了ACEI/ARB对房颤合并高血压患者死亡率的影响。ACEI 和 ARB具有明确降压作用,尤其适用于伴有心力衰竭、心肌梗死后、糖尿病、慢性肾脏疾病的患者,有充足证据证明可改善预后。
其中,ARB 类药物种类繁多,常以「沙坦」命名,包括缬沙坦、氯沙坦、厄贝沙坦、替米沙坦、坎地沙坦、奥美沙坦和阿利沙坦,这7种沙坦类药物均可安全有效的降压。
其中,厄贝沙坦降压幅度较大,单药控制血压的达标率较高,吸收度高,药效持续时间长,在治疗高血压中占有重要地位。

在这项多中心前瞻性研究,研究人员收纳了来自2008 年 11 月至 2011 年 10 月期间,来自中国 20 个急诊中心的 2016 名急诊患者,评估分析了1110 名房颤合并高血压患者。同时,研究人员根据是否接受 ACEI/ARB 治疗对患者进行分组:ACEI/ARB组和非ACEI/ARB组,以评估全因死亡、心血管死亡、卒中和主要不良事件在内的临床结局。
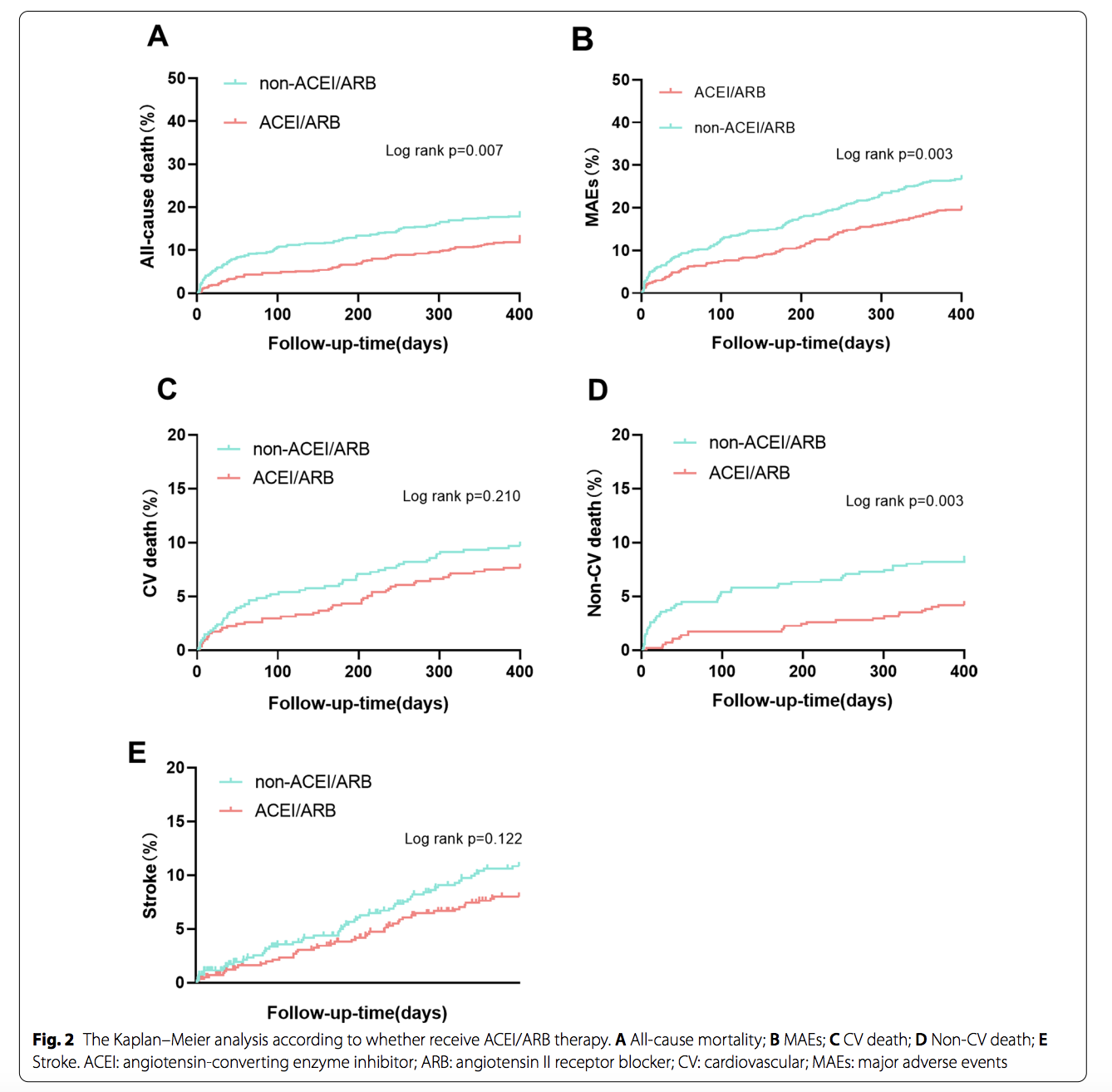
结果显示,在随访1年后,169例患者全因死亡(15.2%)、100例患者心血管死亡(9.0%)和255例患者发生了不良事件(23.0%),而98名患者患了中风(8.8%)。
根据多变量 Cox 回归分析,接受ACEI/ARB 治疗的患者与全因死亡风险降低显著相关,全因死亡率分别为12.5%和18.1%,而且接受ACEI/ARB治疗的患者的发生不良事件的概率更低。然而,两组患者的心血管死亡和中风风险是相当的。
另外,研究人员发现,房颤合并高血压患者的死因多以心衰为主,其次是感染。有趣的是,ACEI/ARB组与感染引起的死亡率明显较低。

在调整混杂因素后,ACEI/ARB治疗与心血管死亡和不良事件发生风险降低显著相关,而ACEI/ARB对卒中的影响是中性的。在单变量和多变量Logistic回归都表明,使用ACEI/ARB与预防阵发性房颤复发之间没有明显的关联。
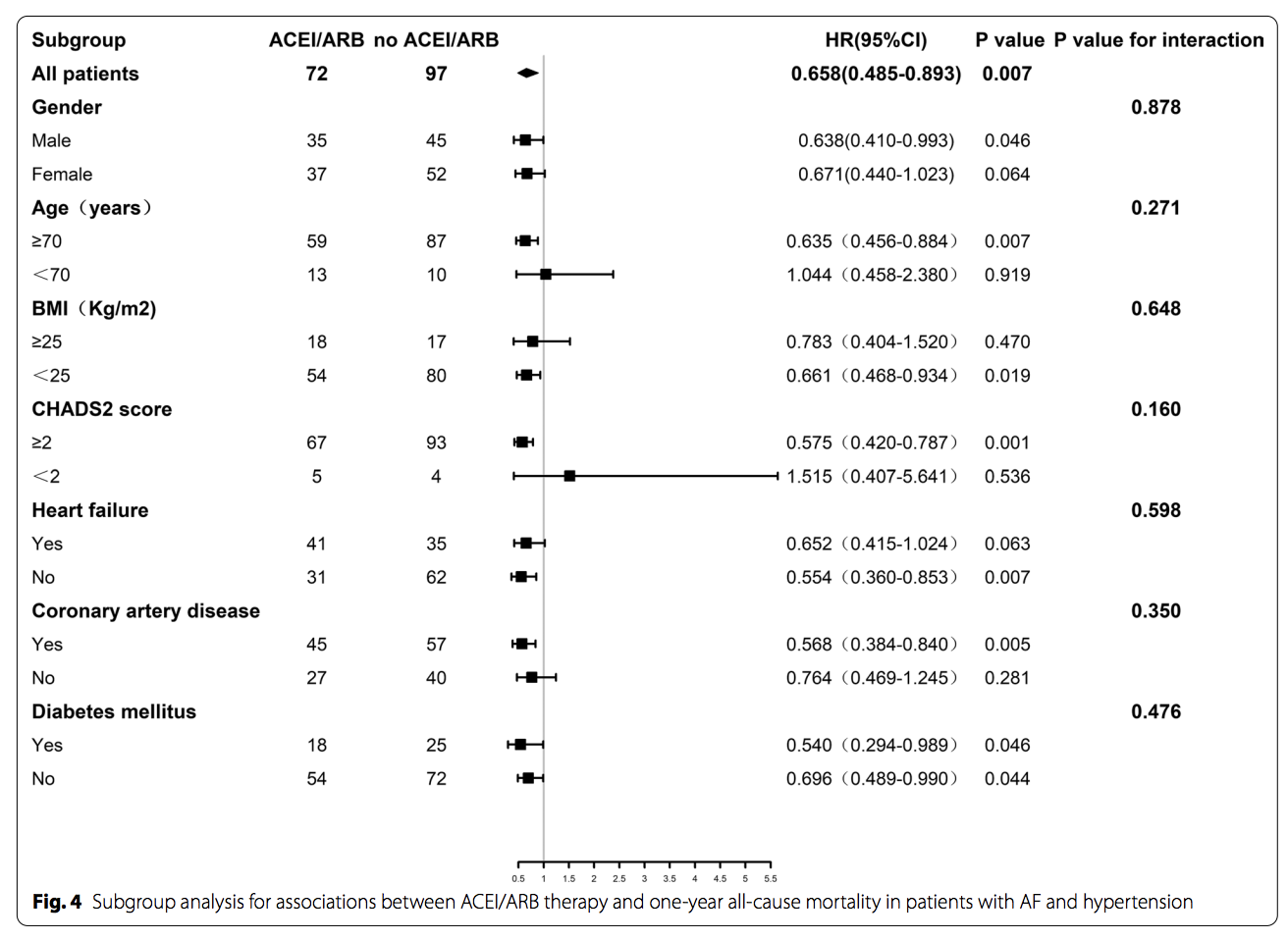
总之,该队列研究的结果表明,接受ACEI/ARB治疗的房颤合并高血压患者的全因死亡和不良事件的发生率较低,特别是在调整了潜在的混杂因素。此外,多变量Cox回归分析结果显示,ACEI/ARB治疗与全因死亡、心血管死亡和不良事件发生风险的降低独立相关。
这些发现表明,除了血压控制治疗外,预防 RAAS 系统的激活可能会改善房颤和高血压患者的预后。这些结果为房颤合并高血压患者的三级预防治疗提供了证据。
原始出处
Xu, W., Yang, Ym., Zhu, J. et al. Impact of renin–angiotensin–aldosterone-system inhibitor drugs on mortality in patients with atrial fibrillation and hypertension. BMC Cardiovasc Disord 22, 141 (2022). https://doi.org/10.1186/s12872-022-02580-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#患者死亡#
52
学习了
34
很受教育
47
#降压#
52
#高血压患者#
37
很受益
35