CHEST:儿童扁桃体切除后阻塞性睡眠呼吸暂停得到缓解?
2015-11-04 MedSci MedSci原创
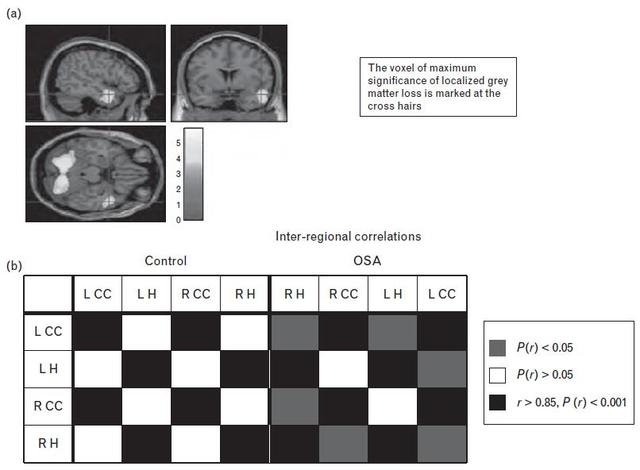
扁桃体切除术(AT)是治疗儿童阻塞性睡眠呼吸暂停综合征(OSAS)常见的方法,但很少有人知道没有治疗的预后。儿童扁桃体切除术试验(CHAT)随机分配合50%的符合条件的OSAS儿童患者作为对照组(观察等待),并进行7个月的症状随访,身体检查和多导睡眠监测。多导睡眠图及对症解决由呼吸暂停/低通气指数(AHI)<2和阻塞性呼吸暂停指数(OAI)<1,以及OSAS症状评分分别定义(小儿睡眠问
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#阻塞#
25
#Chest#
33
#睡眠呼吸#
34
#EST#
34
#扁桃体切除#
28
#呼吸暂停#
28